A group of researchers led by Osaka University established a new pathological grading system to evaluate the therapeutic effect of neoadjuvant chemotherapy (NAC) for metastatic lymph nodes (LNs) removed in esophageal cancer (EC) surgery, demonstrating that the system predicts recurrence and prognosis in EC patients better than conventional systems. Their research results were published in Annals of Surgery.
The majority of patients with progressive EC have LN metastases. Such patients usually receive NAC before surgery. Since patients who showed good response to NAC are known to have a favorable prognosis, it is important to accurately evaluate the therapeutic effect of NAC.
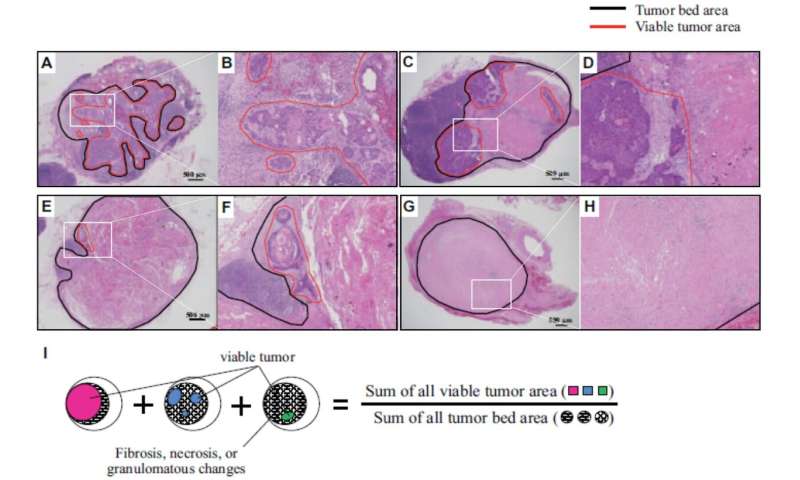
Routine pathological evaluation of NAC is conducted for the therapeutic effect on the primary tumor (PT). PT regression grade is determined by calculating the proportion of viable tumor area within the whole tumor bed area. Evaluations are classified into four categories according to the proportion. A high grade shows a high therapeutic effect of NAC. This tumor regression grade classification is a good indicator for predicting recurrence and prognosis.
Because metastatic status of LN, which is known to be associated with systemic micrometastases,serves as a more reliable indicator ofpatient survival compared with PT progression in EC patients, this grouphypothesizedthat, in patients who have undergone NAC for EC, the pathological LN response might be a better prognostic factor than the pathological PT response.
Among 371 eligible patients, 52 had negative LNs with no evidence of regression. The researchers evaluated the therapeutic effect of NAC for the remaining 319 patients by grading pathological tumor regression into four categories according to residual tumor per tumor bed.
For all metastatic LNs, the researchers generated a total LN regression grade according to the proportion of the summed viable tumor area relative to the summed tumor bed area (Figure 1I). 153 patients (48.0%) exhibited better response and 191 (59.9%) showed a difference in response between the PT and LN regression grades. Specifically:
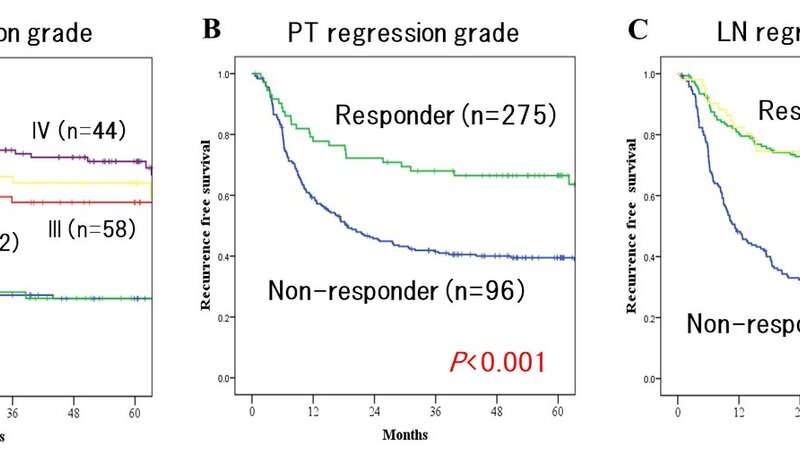
- Prognosis varied depending on the total LN regression grade (Figure 2A) and the recurrence-free survival (RFS) rate among responders was significantly better than that of non-responders.
- Although the therapeutic effect was significantly correlated with survival in both PT (Figure 2B) and LN (Figure 2C), the survival difference was more prominent in LN than PT.
- LN regression grade was an independent prognostic factor of the duration of survival.
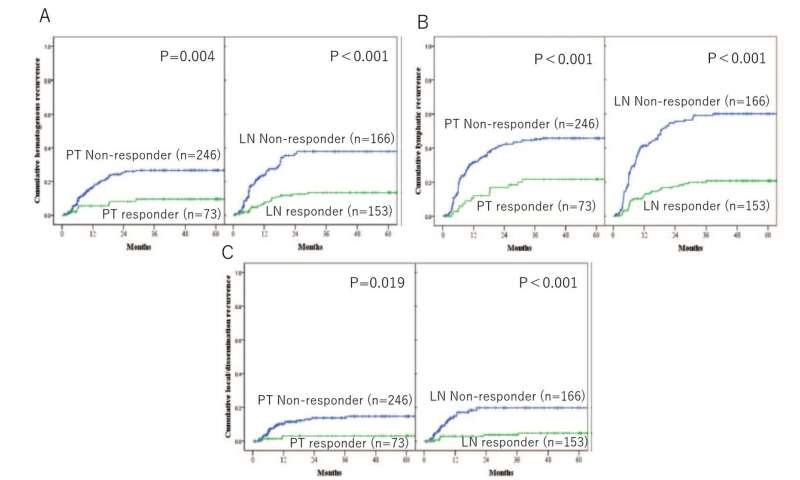
- The rates of hematogenous recurrences and lymphatic recurrences were significantly lower in responder compared with non-responder in both PT and LN. However, these differences were more remarkable in LN response.
These findings show that pathological assessment of all metastatic LNs is excellent in predicting prognosis and disease recurrence in patients who undergo NAC for EC.
Source: Read Full Article
