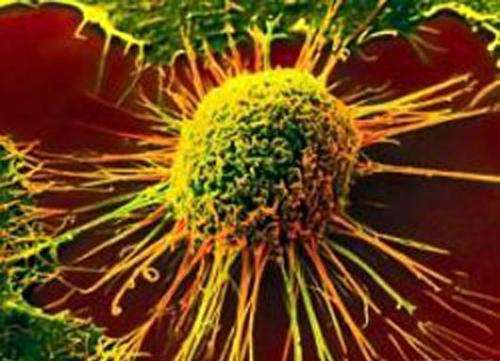
Researchers at the Indiana University Melvin and Bren Simon Comprehensive Cancer Center have identified a target for colorectal cancer immunotherapy.
Immunotherapy uses the body’s immune system to target and destroy cancer cells. Considered the future of cancer treatment, immunotherapy is less toxic than chemotherapy. Colorectal cancer is the third most common cancer among men and women, yet chemotherapy remains the standard of care as limited numbers of patients respond to current immunotherapy treatment options.
The findings published May 7 in JCI Insight could provide additional treatments for a larger number of colorectal cancer patients via a new immunotherapy pathway. Researchers identified ST2 as a novel checkpoint molecule that could help T cells become more effective.
The research is a collaboration between IU School of Medicine cancer researchers Xiongbin Lu, Ph.D., Vera Bradley Foundation Professor of Breast Cancer Innovation and of Medical and Molecular Genetics, and Sophie Paczesny, MD, Ph.D., Nora Letzter Professor of Pediatrics and of Microbiology and Immunology.
Immune checkpoints are an essential part of the immune system with the role of preventing immune cells from destroying healthy cells. T cells are immune system cells that attack foreign invaders such as infections and can help fight cancer. But cancer is tricky, and often the tumor microenvironment creates ways to prevent T cells from attacking cancer cells by misusing several factors including the activation of checkpoint molecules.
Within the tumor microenvironment, the body’s immune system knows something is wrong and sends a stress signal such as the alarmin IL-33, which brings in immune cells called macrophages that express ST2 (the receptor for IL-33) to help. What is at first a “good” response is quickly overwhelmed and the macrophages become the enemy in fighting colon cancer.
The authors investigated using patient tumor genetic data and found that T-cell functionality, one of the key factors in fighting the cancer using the adaptive immune responses, is reduced in patients displaying high ST2 levels. Using tumor tissue samples from IU Simon Comprehensive Cancer Center tissue bank, researchers found abundant expression of ST2 in macrophages in tumor tissue samples from early to late-stage colorectal cancer.
“In all of the patient samples, we were able to identify ST2 expressing macrophages, which would potentially mean that targeting these ST2 macrophages would be relevant to the patients,” Kevin Van der Jeught, Ph.D., said. Van der Jeught is a post-doctoral researcher in Lu’s lab and first author of this study.
In preclinical mouse models, researchers found that by targeting the ST2-expressing macrophages, they were able to slow tumor growth. By depleting these inhibitory cells, the T cells became more active in fighting cancer.
Research collaborator and scientist at the Herman B Wells Center for Pediatric Research, Paczesny’s previous research led to the discovery of ST2 and is the subject of her National Cancer Institute “Cancer Moonshot” grant focusing on immunotherapy for pediatric acute myeloid leukemia (AML). While leukemia and colorectal cancer are very different diseases, researchers have found commonality and collaboration in the ST2 protein.
“This research is bringing together the pathway in two different diseases,” Paczesny said.
Lu’s research focuses on cancer cell biology in diseases such as triple negative breast cancer and colorectal cancer.
“We have to develop new tools and new approaches for solid tumors, and this is the kind of collaboration we need for advancing future treatments,” Lu said. Researchers from two other institutions, the University of Maryland’s Marlene and Stewart Greenebaum Comprehensive Cancer Center and the VIB-UGent Center for Inflammation Research in Belgium, have contributed to this publication.
Researchers also are exploring combination therapy with existing immunotherapy, such as PD-1 checkpoint inhibitors, which work to boost T cells directly, while attacking ST2 on macrophage cells increased T cells by stopping the inhibitors.
“Potentially through a combination of two checkpoints at work on different immune cells, we could enhance the current response rates,” Van der Jeught said.
Source: Read Full Article
