For patients with solid cancers, endoscopic surgery is one of the primary treatment options to remove tumors. However, there is a high risk of cancer recurrence if even a small number of cancerous cells are left behind after surgical resection. To prevent this from happening, researchers developed fluorescence-guided surgery (FGS). In FGS, patients are injected with a fluorescent probe that preferentially binds to tumor cells, enabling surgeons to easily identify lesions with the help of specialized endoscopes that emit the necessary excitation light.
Unfortunately, tumors can be highly heterogeneous, and a single fluorescent probe is not enough to detect them all. Thus, one of the frontiers in FGS is using cocktails of multiple fluorescent probes (a.k.a. “tracers”) to detect a wider range of tumors, as well as to reduce false positives and negatives. Despite some progress in this direction, clinically approved endoscopes are all optimized to detect only a single tracer. Moreover, multi-tracer instruments currently under development are bulky because they require multiple imaging sensors and optical components.
In a study recently published in Journal of Biomedical Optics (JBO), a research team from University of Illinois Urbana–Champaign reported a novel endoscopic imaging system whose design could greatly accelerate the adoption of multi-tracer FGS.
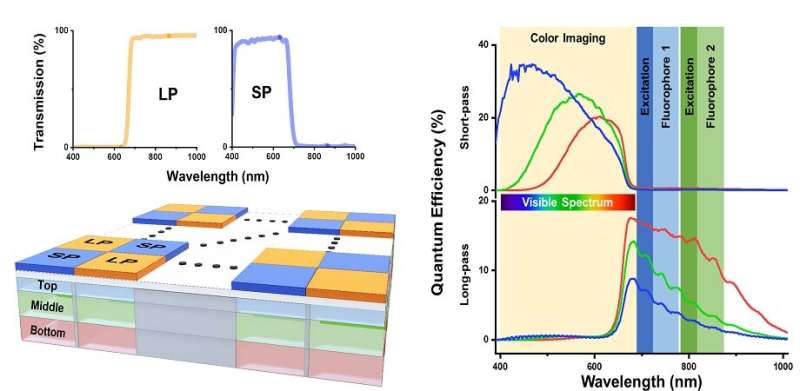
At the heart of this design lies an innovative hexa-chromatic bioinspired imaging sensor (BIS), which the researchers modeled based on the visual system of the mantis shrimp. The sensor consists of three layers of vertically stacked photodetectors covered with a checkerboard-like arrangement of two different filters; one filters visible light and the other filters near-infrared (NIR) light.
The result is a single-chip camera that can effectively capture light on six different spectral channels, thereby making it capable of detecting even the most subtle differences in fluorescence emission from the tissue being imaged. To put its performance into perspective, this BIS can differentiate fluorescent tracers with emission peaks that are just 20 nanometers (nm) apart. Such a feat is not possible with current clinically approved imaging instruments.
To be able to use the BIS effectively, the researchers also had to design an appropriate excitation light source for activating the fluorescent tracers. To this end, they used custom bifurcated optical fibers connected to three independent light sources—a white LED and two NIR lasers at 665 and 785 nm. The researchers coupled the combined output of the fibers at the start of the rigid endoscope. In this way, by using a single imaging sensor and a single light input, they made the device less bulky than other multi-tracer imaging systems.
The researchers conducted characterization and benchmarking tests to determine the spatial resolution and sensitivity of the device. In addition, they performed in vivo experiments on a mouse model for breast cancer. These mice were injected with a 680-nm tracer, an 800-nm tracer, or an equal mixture of the two. The proposed system could clearly differentiate between the fluorescence signatures produced by the individual tracers and the mixture.
Aiming to showcase the clinical potential of their endoscope, the researchers used it to image lung cancer nodules that had been just removed from patients. Although these patients had only been injected with one fluorescent tracer, the proposed device was still capable of accurately distinguishing malignant nodules from healthy tissue.
Overall, the researchers achieved important engineering breakthroughs that will pave the way to the adoption of multi-tracer FGS. Thanks to its higher spatial resolution and its remarkable capacity to detect small variations in fluorescence emission, the proposed endoscopic imaging system will help doctors detect smaller or otherwise hidden tumors more easily.
More information:
Mebin B. George et al, Bioinspired color-near infrared endoscopic imaging system for molecular guided cancer surgery, Journal of Biomedical Optics (2023). DOI: 10.1117/1.JBO.28.5.056002
Journal information:
Journal of Biomedical Optics
Source: Read Full Article
