After three school years disrupted by COVID-19, parents, teachers, and kids just want the new one to be… normal. Or as close to it as possible.
And thanks to vaccines, tests, medicines, and better knowledge, that goal might be closer than ever.
But it won’t happen automatically.
That’s why the Centers for Disease Control and Prevention, and the United States Food and Drug Administration, both just updated their national guidance on what schools and individuals can do to reduce COVID-19’s impact this school year.
“At this point in the COVID-19 pandemic, we need to take a universal approach to wellness,” said Laraine Washer, M.D., Clinical Professor of Infectious Disease and the hospital epidemiologist at Michigan Medicine. “Given the occasionally deadly outcomes of this virus, we all have a responsibility to avoid being around others outside your household when we are sick.”
Here are six things families and educators can do now, and throughout the school year, to give kids a learning experience that’s as normal as possible.
1. Get all the protection you can from vaccines.
Kids and teens who haven’t gotten vaccinated, or who got vaccinated but haven’t yet gotten a booster dose of vaccine should get one as soon as possible.
Last week, the FDA and CDC approved new bivalent booster shots, which offer better protection against the Omicron BA.4 and BA.5 variants that are currently circulating. These shots will be offered as a Fall booster:
-
It is recommended that those 12 years and older who received their primary series or prior monovalent booster dose at least 2 months previously should get the new bivalent COVID booster vaccine. Those 18 and older can get either Pfizer or Moderna bivalent booster. Those 12-17 years can only get the Pfizer bivalent booster.
-
Children 5-11 years who have had their primary series but have not had a booster dose are only eligible for the older vaccine booster
And do not forget the younger siblings of school-age children. Safe and effective COVID-19 vaccines are available for kids as young as six months old.
Studies have shown that vaccinated kids and adults, and especially those who had been boosted, tend to have less severe symptoms.
Back-to-school time is also a time to make sure children and teens are up to date on their other vaccines, especially if they missed regular doctors’ appointments in the last two and a half years.
Mark your calendar to get everyone over the age of 6 months vaccinated against flu this fall. Down in Australia, where the flu circulates during their winter while Americans are enjoying summer, it’s been an especially bad flu season. That could mean this winter will bring bad flu to the U.S.
2. Use masks wisely.
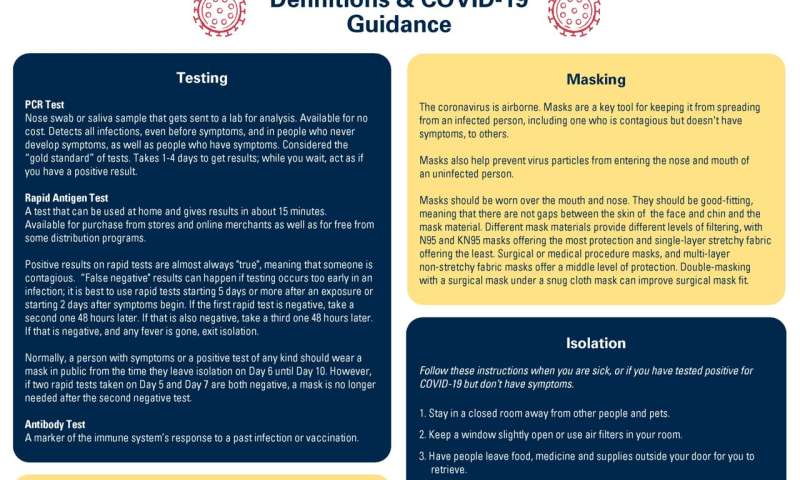
Masks continue to protect against COVID-19, including new against new variants that can sneak around the immune system.
The new CDC guidance recommends schools require masks any time the surrounding community’s level of COVID-19 is at “High.” And it says that anyone wishing to wear a mask in school when levels are lower should receive support.
Your back-to-school shopping list should focus on higher-filtration masks. If your child is struggling to wear a well-fitting surgical or higher filtration mask such as a KN95, KF94, or N95 masks, a cloth mask is better than nothing. The best mask should be well-fitting and comfortable enough for your child to wear throughout the day.
Other mask recommendations:
-
Even if a school doesn’t require masks at “High” community levels, talk to children and teens about how voluntarily masking when there’s a lot of COVID in the community could keep them from getting sick and having to miss school.
-
Anyone who lives with or has been a close contact of a person who has COVID-19 should also mask in public for 10 days.
-
Masks may be required in classrooms where high-risk kids are learning; see the section below.
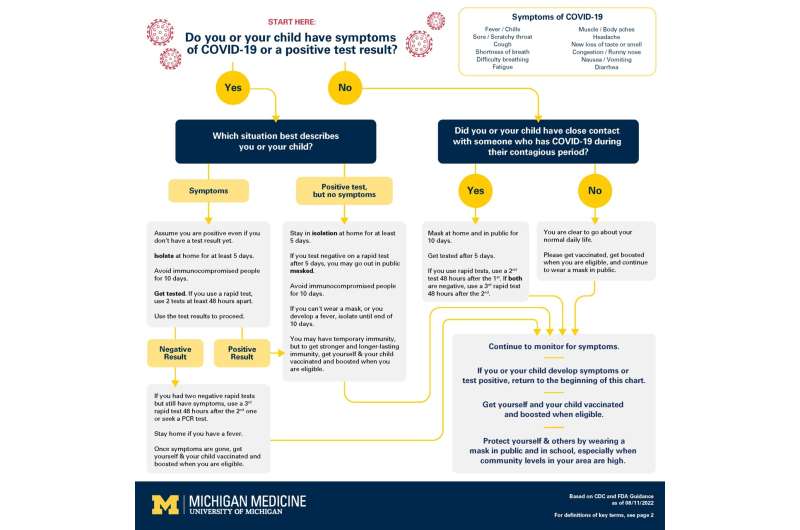
This advice hasn’t changed: people with fevers or other potential symptoms of COVID-19 should stay home, in isolation, until at least five days have passed and fever is gone for 24 hours without the help of medicine.
Isolating means separating the infected person from the rest of the household in a closed room, bringing them food and drink to leave outside their door, and requiring them to wear a mask if they have to come out to use a bathroom. Learn more about isolation.
Some individuals who are immunocompromised may need to isolate or wear a mask longer and or have negative rapid antigen tests twice in a 48-hour period to end isolation.
People who had shortness of breath or were hospitalized for COVID-19, or who have an immune system that’s been weakened by a condition or medication, should isolate for the full 10 days.
4. Protect kids and adults at higher risk of severe illness.
Even healthy young people can develop severe cases of COVID-19. But some children and adults have a much higher risk of severe illness if they catch the virus.
The new guidance gives ways to protect them, including:
-
Children with health conditions and disabilities have special protection under education law to ensure they have access to equal educational opportunities, and schools must make reasonable accommodations for them. The U.S. Department of Education has guidance for how this relates to COVID-19. Parents and guardians of children who have conditions that put them at higher COVID-19 risk should talk to their school, even if they don’t currently have an Individualized Education Program or Section 504 plan.
-
Everyone who lives with someone who has a high risk of severe COVID-19 because of their health or age should take extra precautions (such as masking in school and public places) when community levels are at CDC’s High level.
-
If you’re planning to visit a high-risk person, use masks and rapid tests to reduce the chance you’ll bring COVID-19 to them, especially if your child is in school or activities where they aren’t wearing a mask regularly. Anyone who recently had COVID-19 should wait until at least the 11th day after symptoms started to visit a high-risk person.
-
Anyone over age 12 who has an increased risk of severe COVID-19 may qualify to receive medications such as Paxlovid if they get the disease, but these must be started within the first five days after the illness begins. Talk to a pharmacist or health provider.
-
For very high-risk people over the age of 12, a preventative antibody (Evusheld) directed against COVID-19 is available. Evusheld is a monoclonal antibody that can prevent severe disease and is given every six months to people at very high risk for severe COVID-19. Examples of people who could benefit from preventative antibodies are people in chemotherapy, or taking high-dose steroids or other immune-suppressing medications.
More fresh air, and more filtration of indoor air, can help reduce COVID-19 spread in schools and other settings.
Ask what your school leaders are doing to improve air quality, and whether they’re following the CDC’s current recommendations.
Opening windows, using high-quality filters on the central heating and air conditioning system, increasing the percentage of fresh air that gets mixed into that central air supply, and putting devices that filter the air in classrooms, are all ways to get any virus out of the air that children and teachers breathe. Filters should be regularly cleaned or replaced.
6. Have rapid tests on hand and know when to use them.
For most of the last school year, rapid tests were hard to find in stores and other locations. But now they’re plentiful, health insurance plans must cover their cost up front or after purchase, and the federal government and some states including Michigan offer them for free.
Now’s the time to stock up on tests during back-to-school preparations, so you have them handy.
If someone has symptoms and tests positive on a rapid test, it’s almost certain that they have COVID-19 and could spread it to others. They should go into isolation for at least five days after the day of their first positive rapid test.
Particularly for vaccinated people, symptoms can show up a few days before the rapid tests return positive.
That’s why new FDA guidance says that if someone has COVID-19 symptoms or a recent close contact, and they test negative on a rapid test, they should test again with another rapid test 48 hours later. (During those 48 hours, they should go into isolation if they have symptoms, or wear a mask in public if they’ve had a close contact. They could also go get a PCR test which is more accurate early in an infection.)
If that second rapid test is also negative, the FDA says they should do a third one 48 hours later—and continue to follow CDC guidance to isolate or mask in the meantime.
On the other hand, rapid tests are highly accurate after someone has been sick for a while. That’s why new CDC guidance allows the use of rapid tests toward the end of COVID-19 illness to see if it’s safe for a person to go out in public without a mask. (Remember that they shouldn’t go to school or out in public at all until the sixth day after their symptoms started, and only if any fever has been gone for 24 hours.)
If someone is recovering from COVID-19 and their fever is gone, they can use a rapid test on the fifth day after symptoms started, and then another one 48 hours later on the seventh day. If both tests are negative, they can then go in public or to school without a mask, as long as that’s allowed by their school.
Source: Read Full Article
