A collaborative effort between investigators at Roswell Park Comprehensive Cancer Center and the Center for Molecular Immunology (CIM) in Havana, Cuba, has revealed a new strategy for correcting immune dysfunction in cancer patients. Findings from this research, which involved both laboratory studies and an early-phase clinical trial, show that a novel immune modulator known as VSSP can significantly reduce myeloid-derived suppressor cells (MDSCs) among individuals with advanced kidney cancer.
This work, recently published in the Journal for ImmunoTherapy of Cancer, opens the door for the development of an immune-modulating therapy that could overcome immune dysfunction—in this case, an overproduction of MDSCs that can aid the progression of cancer—creating more favorable conditions for generating an antitumor response.
“While it is well-appreciated that the immune system can be effective against cancer, we also know that the effectiveness of existing therapies may be hampered by counter networks of immune suppression,” says Scott Abrams, Ph.D., senior author on the new work and Distinguished Member and Professor of Oncology in the Department of Immunology and Co-Leader of the Cancer Center Support Grant (CCSG) Tumor Immunology and Immunotherapy Program at Roswell Park.
Previous research has shown that antitumor immune responses can be improved by blocking MDSCs—a prominent cell type that drives immune suppression. Those approaches have shortcomings, though, because they address limited aspects of MDSC biology.
The investigators sought to find an alternative method for targeting MDSCs using VSSP, which stands for “very small size particle,” and is a novel immune modulator developed by the CIM team. VSSP is a nanoparticle that has been in clinical development in Cuba for more than 10 years and has been incorporated into the formulation of three different cancer vaccine candidates currently at different stages of clinical testing, including phase 3 trials.
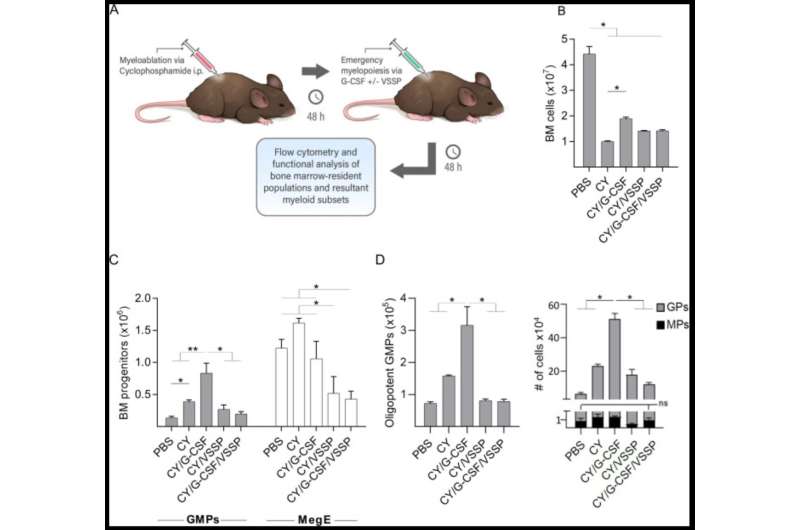
The team focused on the concept of differentiation, which enables cells to mature. Since MDSCs comprise populations of immature cell types, the team tested whether this agent drives MDSC maturation as a means to reduce their burden. In the new publication, the investigators demonstrate that the administration of VSSP in preclinical models drove MDSCs in the bone marrow to become monocytes and dendritic cells—an outcome that carries potential merit for treating cancer patients with high MDSC burden.
As part of the new study, investigators at the CIM also completed an early-phase clinical trial of VSSP in 15 patients with metastatic kidney cancer. Following treatment with VSSP, the number of MDSCs in patients’ blood was significantly reduced, accompanied by increased levels of monocytes and dendritic cells, as observed in the preclinical studies.
“Together, these clinical and preclinical findings strengthen the evidence that VSSP can be used to correct myeloid dysfunction in cancer, and also provide a rationale for combining VSSP with other immuno-oncology agents,” says study co-senior author Jason Muhitch, Ph.D., Assistant Professor of Oncology in the Department of Immunology and Co-Leader of the Genitourinary Cancer Translational Research Group at Roswell Park.
“Our findings also suggest that the mechanism by which VSSP is interfering with the immunosuppressive signals coming from the tumor is at early stages of the generation of the myeloid dysfunction,” adds Circe Mesa, Ph.D., of the Department of Immunoregulation, Immunology and Immunotherapy Direction at the CIM. “This may position VSSP as a first-in-class immune-modulating therapy to combine with antitumor therapies dampened by a dysfunctional myeloid compartment.”
Source: Read Full Article
