Bone injury is common in clinics, and critical-sized bone defects cannot be self-healed. The “gold standard” of clinical treatments for such defects is still dependent on the transplantation of autologous/allogeneic or artificial bone grafts. However, there are flaws, such as donor limits, immune rejection, infection risk and poor osseointegration, which may eventually lead to secondary surgery due to heterogeneous scar regeneration, delayed healing or even nonunion. Despite the prevalence of regenerative strategies based on bioactive materials and stem cell transplantation, the full-thickness reconstruction of critical-sized calvarial defects remains challenging.
An alternative strategy is the in situ delivery of soluble factors by recruiting and empowering endogenous stem/progenitor cells for more efficient tissue repair. Indeed, harnessing endogenous stem cells by recombinant growth factors for tissue regeneration has been extensively studied, and it can avoid the complicated process of extraction, purification, amplification, and quality control required for exogenous stem cell transplantation. While the in vivo stem/progenitor cells during the bone regeneration process are also highly heterogeneous, biomedical engineering strategies using soluble factors by targeting the in situ expansion of specific stem cell subpopulations with osteogenic potential remain challenging.
To overcome these obstacles, the research team led by Prof. Ouyang Hongwei at Zhejiang University School of Medicine developed a 3D-printed hydrogel scaffold incorporated with a cocktail of optimized NSs for use as an in situ cell culture system, which not only induces the robust expansion of MSCs in vitro but also achieves a full-thickness regeneration of critical-sized calvarial defects in vivo. This study was published in Nature Communications.
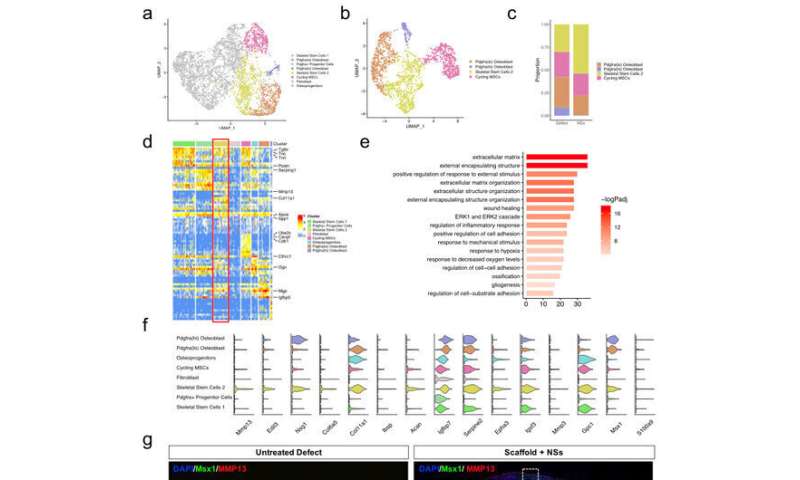
Notably, by single-cell RNA analysis, they found that the implantation of the culture system can greatly promote the in situ recruitment and expansion of a specific Msx1+ skeletal stem cell (SSC) subset. Moreover, the enhanced bone regeneration is accompanied by endochondral ossification closely correlated with Msx1+ skeletal stem cell (SSC) subset. This study illustrates the time-saving and regenerative efficacy of in situ stem cell expansion by a tissue engineering scaffold containing soluble factors for more efficient bone regeneration.
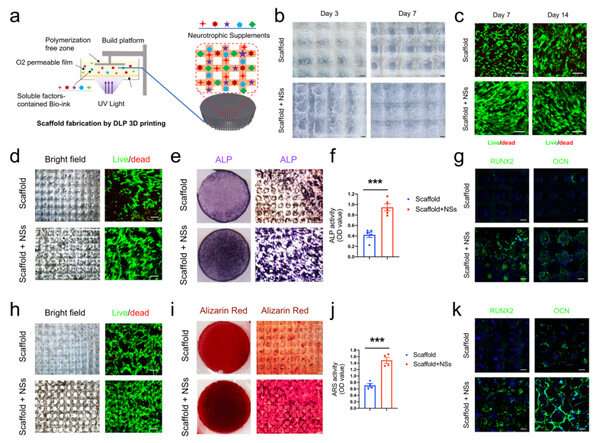
By using digital light processing (DLP) 3D printing technology, Prof. Ouyang and his team fabricated a NSs-incorporated 3D hydrogel culture system. The results showed that with NSs in the medium, MSCs were apparently expanded and densely attached across the pore structures. This provides some theoretical basis for the in situ expansion and osteogenic differentiation of endogenous stem cells.
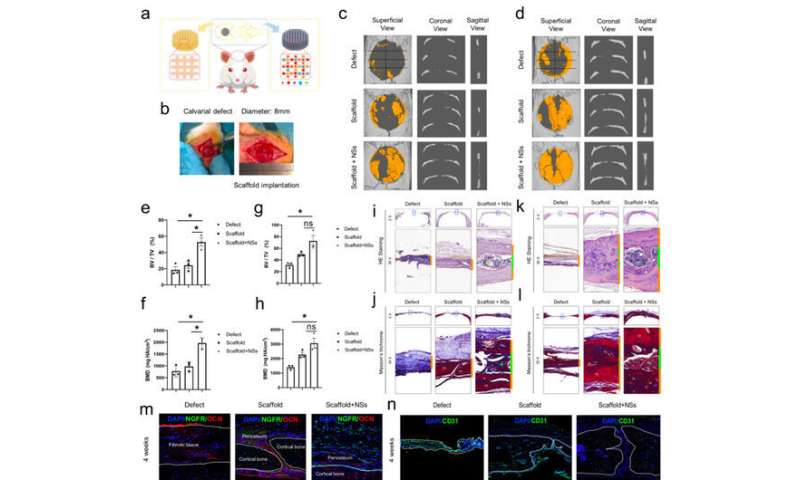
To evaluate the potential of the local delivery of NSs for promoting bone regeneration, the researchers tested the effect of their in situ transplantation on the full-thickness regeneration of critical-sized calvarial defects. The results demonstrated that the local delivery of NSs can significantly restore the integrity of the full-thickness calvarial structure and promote its functional regeneration.
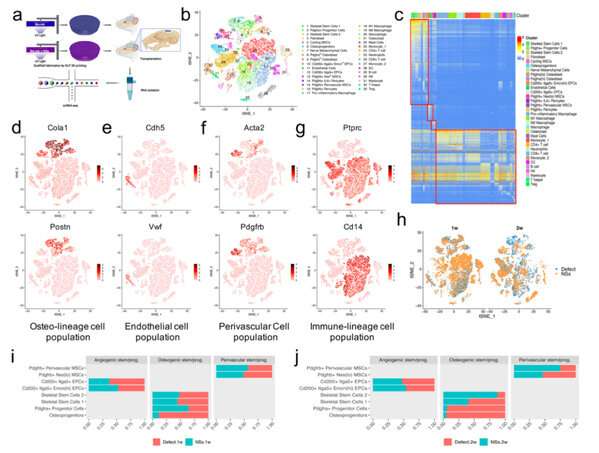
Through single-cell RNA-sequencing analysis, they discovered that specific tissue engineering grafts can regulate the profiles of specific regenerative cell subpopulations during bone injury repair, which provides a reasonable cellular mechanism for the repair of bone defects.
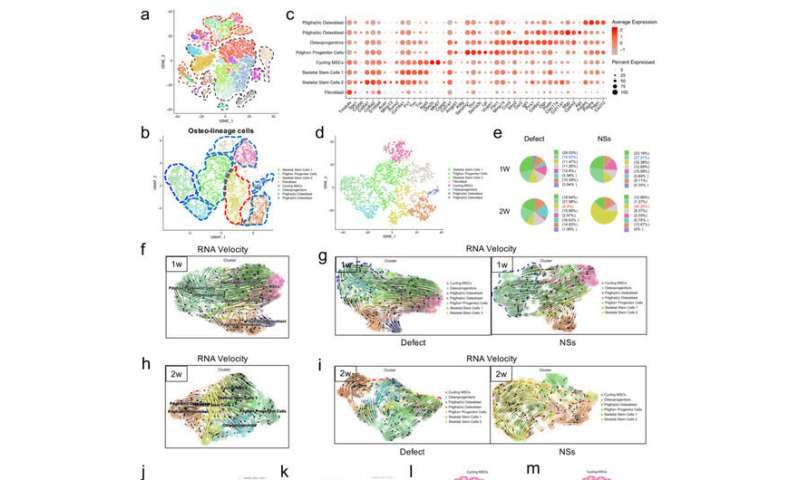
Notably, cellular composition and tissue staining showed that the local insertion of this NSs-containing in situ cell culture system can remarkably expand the Msx1+ SSCs subset during bone regeneration. In addition, the differentiation trajectory demonstrated a molecular feature of Msx1+ SSC2 that underwent the endochondral pathway, suggesting that Msx1+ SSC2 acquired an endochondral bone formation capacity for injury repair, rather than a direct intramembranous ossification.
Source: Read Full Article
