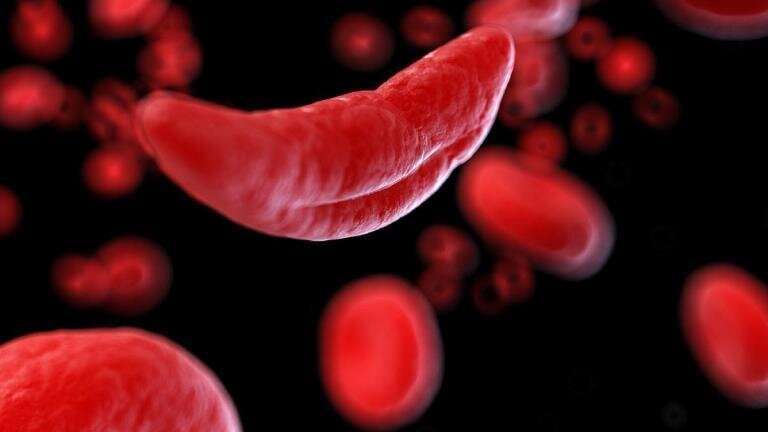
A new study suggests the number of deaths due to sickle cell disease is 11 times higher than what is indicated from mortality data sources alone. Sickle cell disease is not just underdiagnosed, but it also increases risk of infection and of death from conditions like stroke, heart problems, kidney problems, and pregnancy complications.
This means that the doctor taking care of a sickle cell disease patient who died from stroke may not even know that person had sickle cell disease or may not know that sickle cell disease can cause stroke, both of which could lead the doctor to not list sickle cell disease as a cause of death for that person.
When other sources of data on prevalence and birth incidence were combined with mortality data in epidemiological modeling, in 2021, the “total mortality burden” of sickle cell disease was 373,000 deaths, compared to 34,600 sickle-cell-only deaths, or “cause-specific deaths.” The increase was especially pronounced in South Asia and sub-Saharan Africa, where the fatality figures were 67 times higher and nine times higher, respectively.
The study analyzed global health data from 2000 to 2021 and is published today in The Lancet Haematology journal. The research is part of the Global Burden of Disease 2021 study coordinated by the Institute for Health Metrics and Evaluation (IHME) at the University of Washington’s School of Medicine.
“Our research reveals the stark reality that sickle cell disease is far deadlier than its textbook description,” says senior author Dr. Nicholas Kassebaum, Adjunct Associate Professor at IHME. “The number of babies born with sickle cell disease is rising, which means a very difficult early childhood. Patients are more susceptible to infections and other severe conditions, so early detection is key for treatment.”
In 2021, half a million babies were born with sickle cell disease, and more than three-quarters of these births were in sub-Saharan Africa. Under the analysis of total mortality burden (including secondary conditions), sickle cell disease was the 12th leading cause of death globally for children under the age of 5 years. However, total sickle cell disease mortality burden was among the top three causes of death in Portugal, Jamaica, Libya, Oman, and San Marino.
“Improved data collection is critical to tracking progress on sickle cell disease. In order to overcome this data limitation, instead of using mortality data alone to estimate total sickle cell disease deaths, we used a mathematical algorithm that also takes input data from birth incidence, survival over time, and prevalence, and ensures these measures are internally consistent,” explains Azalea Thomson, first author and IHME researcher on the Neonatal and Child Health Team.
“By making use of all available data, we were able to strengthen our understanding of the true burden of sickle cell disease and better contextualize it alongside other leading causes of death. For example, in 2021, in kids under 5 years in sub-Saharan Africa, total sickle cell disease deaths exceeded those from malnutrition, measles, or syphilis.”
The research also underscores the need for policymakers and public health advocates to address the largely underrecognized burden of sickle cell disease. Universal newborn screening, case monitoring through public registries, and early intervention treatment can alleviate suffering for some 8 million people living with sickle cell disease.
“Universal newborn screening is essential for early diagnosis and management of sickle cell disease,” says Dr. Theresa McHugh, scientific writer at IHME who focuses on neonatal and child health. “In low- and middle-income countries, the newborn screening process is fragmented. In the US, newborn screening is universal, but a national registry does not yet exist. Increased global awareness and adoption of health policies that expand neonatal screening and make treatment more accessible will go a long way in improving health outcomes.”
More information:
Global, regional and national prevalence and mortality burden of sickle cell disease, 2000-2021: a systematic analysis from the Global Burden of Disease Study 2021, The Lancet Haematology (2023). www.thelancet.com/journals/lan … (23)00118-7/fulltext
Journal information:
The Lancet Haematology
Source: Read Full Article
