Lower back pain caused by degenerative disc disorder affects approximately 40% of the population over 40 and though many of us may never experience adverse effects from the disorder, it is the cause of chronic back pain for numerous Americans. Recent imaging diagnostics and cellular based direct-injection therapeutics for degenerative disc and spinal cord injuries have shown great promise for chronic back pain sufferers, however the targeted area for delivery is very small and narrow, requiring extreme precision by the clinical practitioner to avoid the bony vertebrae and other sensitive tissues.
The normative anatomy of the spinal area is quite complex. Between each vertebra is a ‘disc’ of fibrous cartilage surrounding a sac of gel-like fluid that act as the spine’s shock absorbers, as well as giving the spine flexibility. Primary nerve branches to the various location of the body travel through this area from the central spinal canal. The complexity is increased if the patient has pre-existing conditions such as bone abnormalities due to scoliosis or osteoarthritis, spinal stenosis (a narrowing of the spinal canal causing compression) or have surgical implants, such as plates, rods and screws. Depending on the type of therapy, number of injections required, and the injection positioning complexity, spinal injection therapy treatment time frames can range from ~15 minutes to two hours, excluding post-procedure recovery time.
To increase injection site positioning preciseness, and thus the effectiveness, of these new treatments the Biorobotics and Human Modeling Lab, under the direction of George W. Woodruff School of Mechanical Engineering Professor Jun Ueda, have developed a patient mounted injection needle robot for use in magnetic resonance elastography (MRE), a technology that combines MRI imaging and low-frequency vibrations to create a map (elastogram) that images the stiffness of soft tissues. Working in conjunction with the Stevens Institute of Technology and the Mount Sinai Hospital, the team developed non-ferromagnetic lead zirconate titanate (PZT) actuators that allow for usage in the magnetic field area produced by MR imaging. The team used the prototype in a demonstration MRE scan for improved diagnosis of degenerative disc diseases. Multi-source shear wave propagation for examination of the pathological state of the patient tissue is achieved by tunable resonant frequency of the individual actuators. This allows for a minimally invasive procedure with a significant increase in precision needle positioning than that available via a human clinician.
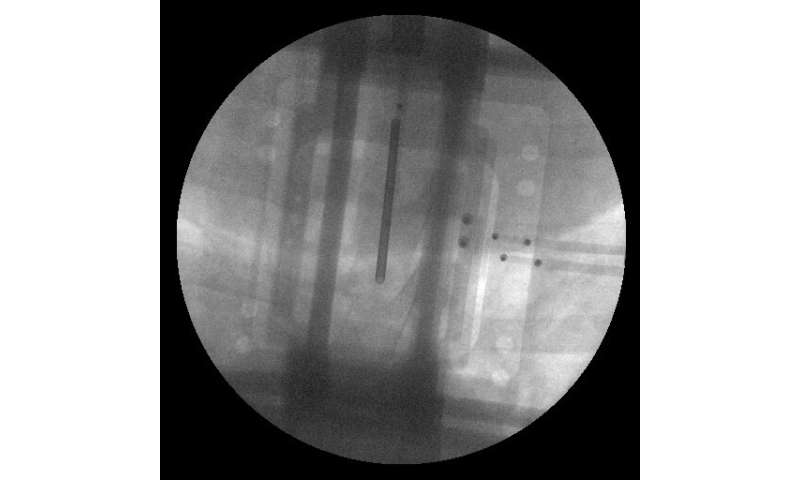
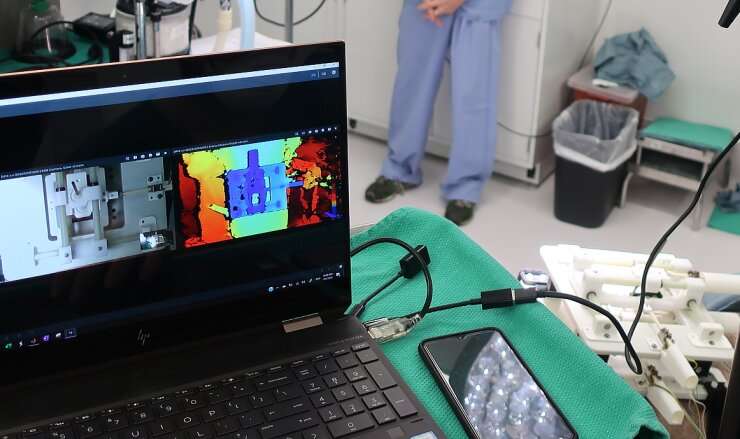
In a related project with Emory University and the Georgia Tech Research Institute, Professor Ueda and team developed a patient mounted, minimally invasive, injection needle robot for spinal cellular therapeutics that is fully MRI compatible due to the non-ferromagnetic materials comprising the robotic actuators. High-precision in-vivo performance has been achieved by a PZT-driven parallel-plane needle-orientation mechanism and an iterative super-resolution computer vision algorithm. Preclinical evaluation on a suidae model showed mounting and controller functionality with respiration, while laboratory evaluation demonstrated placement precision of ~14μm of the desired location.
Source: Read Full Article
