Checkpoint inhibitors have become important tools in the cancer-fighting arsenal. By blocking proteins that normally restrain the immune response, these drugs can help the immune system destroy cancer cells.
But they don’t work in all patients. And now a new study in Nature Immunology led by researchers from Penn’s School of Veterinary Medicine suggests a possible reason why: Not only can these drugs encourage the activity of cancer killing T cells, but they can, in some cases, also activate a population of regulatory T cells that serve the opposing function—to rein in that attack.
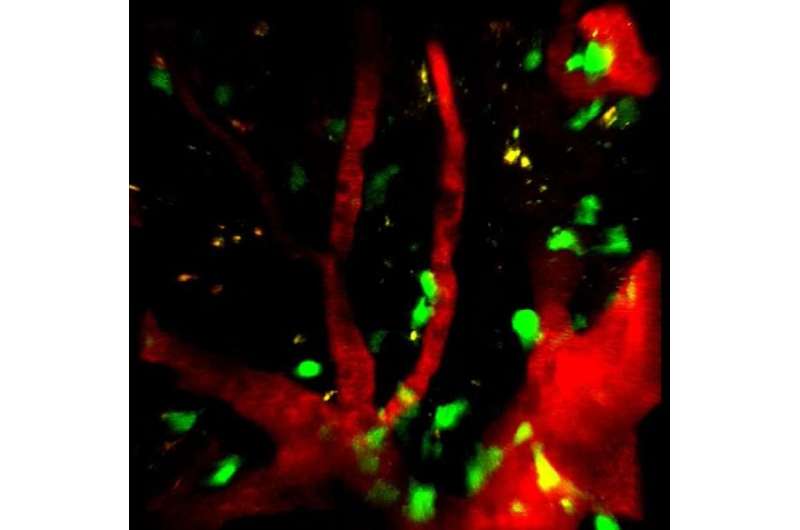
In the study, immunologists led by Penn Vet professor Christopher Hunter and doctoral student Joseph Perry discovered that blocking the activity of the checkpoint protein PD-L1, which interacts with a T cell receptor PD-1, enhanced the activity of a subset of T cells known as effector regulatory T cells, or effector Tregs. This intervention unexpectedly reduced the ability of mice to control a parasite infection.
The findings reveal a complexity to how the body “regulates the regulators” of the immune system, says Hunter. “Once you have those Tregs to control your T cell response, you also need to control them,” he says. “It’s like with a car. You have the ignition, the accelerator, and you also need a brake. PD-1 is a brake not only on killer T cells but also on Tregs.”
T cells may be best known for their roles in fighting infections and killing cancer cells. But the immune system also has several mechanisms in place to counterbalance those responses to prevent out-of-control inflammation that could damage healthy tissue. Tregs are one aspect of this balancing act.
“You can think of Tregs as the health and safety inspectors of the immune system,” Hunter says. “They’re really important, but sometimes, when you need to mount an immune response against a pathogen, you need them to take a back seat. When an infection is present, we see Treg levels crash so that an effector response can emerge. But we never understood what causes that crash.”
The researchers began to understand more after exploring an unanticipated finding. They discovered that, when the checkpoint protein PD-L1 was blocked, mice infected with Toxoplasma gondii were less effective at fighting off the parasite than mice with an uninhibited PD-L1. “That was the opposite of what we expected,” Hunter says, as the dogma would have suggested that blocking this checkpoint inhibitor would allow for a better effector T cell response against infection.
Digging into the surprising result, Perry, Hunter, and colleagues realized that it aligned with what some cancer researchers had recently reported. In certain cancers, the other groups had found, blocking PD-L1 led to worse outcomes, seemingly because of an increase in a population of Tregs that restrained killing of cancer cells.
When the Penn-led team looked in the context of a T. gondii infection, they discovered the signaling molecule interferon gamma turned on PD-L1, which precipitated a rapid decline in Treg numbers. A PD-L1 inhibitor mitigated this effect and stopped the Treg crash. This treatment alleviated the harmful effects of inflammation on mice but also impaired the ability of T cells to fight infection. Similarly, Tregs altered to lack PD-1, the receptor which with PD-L1 interacts, also led to increases in Treg activity.
“It seems that the effector T cell versus Treg ratio is really important,” says Hunter.
As the researchers began to learn more about how Tregs were activated and operated during an infection, they were curious about whether this pathway worked when animals were in a normal, healthy state. Just as there are different types of “regular” T cells, including CD8 and CD4 T cells and many more subdivisions besides, the new work underscores that there are subpopulations of Tregs as well, which have different roles in the body. In healthy, uninfected animals, the team found differences between the proteins expressed by different Treg populations, including some that expressed PD-1, which the researchers termed “effector Tregs.”
“These results taught us that there’s a large population of activated PD-1-positive Treg cells present as a normal part of everyday life that help limit the immune system,” Perry says.
“We think these PD-1 high cells are the most active Tregs,” says Hunter. “It’s a complex landscape, and it’s possible that some checkpoint inhibitor treatments have been inadvertently targeting these Tregs and not others, leading to unexpected outcomes.”
Source: Read Full Article
