An internal medicine clinic at Oregon Health & Science University has sharply reduced the amount of opioids prescribed though innovative use of a review board comprising a team of health care professionals from various disciplines to ensure patients’ needs are being met.
This opioid review board advises OHSU primary care and internal medicine providers seeing patients who had been prescribed powerful and addictive pain-killers.
Their experience was published today in the journal Annals of Family Medicine.
“Once we began to discuss these cases, our numbers really began to come down quite steadily,” said co-author Mary Pickett, M.D., associate professor of medicine (general internal medicine and geriatrics) in the OHSU School of Medicine.
In 2016, the Centers for Disease Control and Prevention adopted a landmark set of opioid-prescribing guidelines. The guidelines, which happened to be co-authored by Roger Chou, M.D., director of the Pacific Northwest Evidence-based Practice Center at OHSU, were intended to ensure patients have access to safer, more effective chronic pain treatment while reducing the number of people who misuse or overdose from opioids.
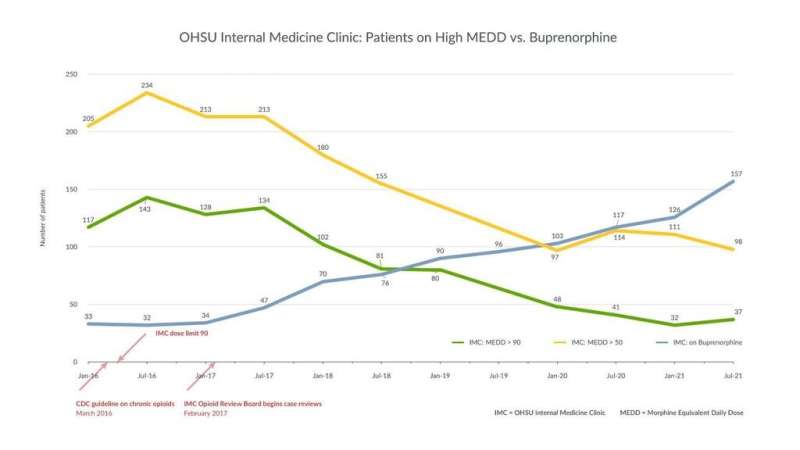
OHSU internal medicine clinicians had been focused on safe prescribing well ahead of the CDC guidelines, but starting in 2017, the board began to systematically review high-risk cases in the clinic.
“The question was, how do clinics actually implement those guidelines in practice?” said Jonathan Robbins, M.D., assistant professor of medicine (general internal medicine and geriatrics) in the OHSU School of Medicine. “The opioid review board was a way to turn high-level recommendations into action steps we can take in our clinic to treat patients and create a culture of safe prescribing.”
Patients sign a waiver to have their treatment reviewed by the board, which meets monthly for an hour and comprises several physicians, a clinical pharmacist, a licensed clinical social worker, a medical assistant, a patient access specialist and a medical resident. The clinic started by reviewing treatment of patients being prescribed more than 90 morphine equivalent daily doses, or MEDD.
The clinic used electronic search methods to review a large volume of patient records.
“We combed through 14,000 patients in our clinic and developed a registry about who we’re chronically treating with opioids,” Pickett said. “We picked out high-risk cases to review and invited those patients’ primary care doctors to consult with us.”
The group initially identified 664 patients on chronic opioid therapy.
Source: Read Full Article
