Dr. Andrew Stokes, assistant professor of global health, is providing mortality data and modeling to the Documenting COVID-19 project and Muckrock in a collaboration that aims to identify the scope of underreported COVID-19 deaths in US counties.
As the United States’ official COVID-19 death toll surpasses 805,000, a Boston University School of Public Health (BUSPH) researcher is partnering with a team of investigative journalists and academics to understand a hidden aspect of COVID-19 mortality: direct and indirect deaths from the pandemic that have not been attributed to COVID-19, and therefore, are excluded from official COVID-19 death totals.
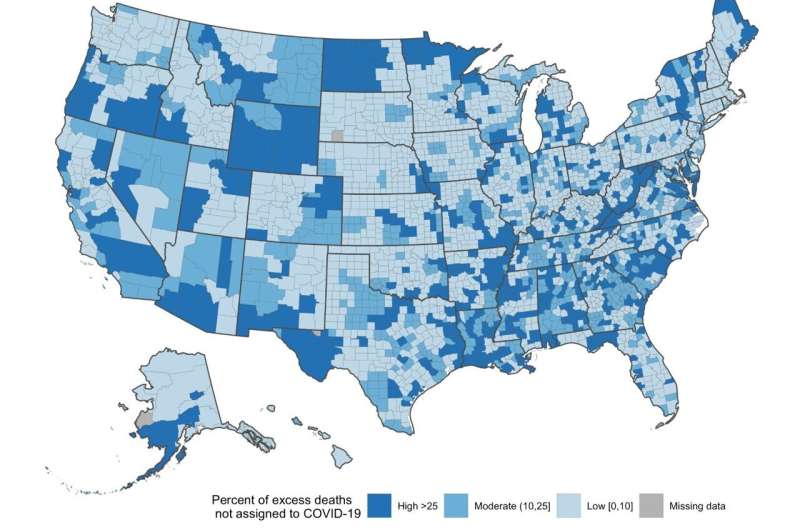
Dr. Andrew Stokes, assistant professor of global health at BUSPH, has studied COVID-19 mortality rates throughout the pandemic, and has conducted several studies that suggest that the true number of COVID deaths in the US is likely much higher than records indicate—and that almost all of the uncounted deaths are occurring at home. These findings show that approximately 20 percent of excess deaths—i.e. the number of deaths beyond what would have been expected in a normal year—were not reflected in COVID-19 death counts among US counties. These hidden deaths appear to occur more often in counties with fewer primary care physicians, less access to health insurance, and more home deaths, and disproportionately among communities of color.
Dr. Stokes is sharing the data and modeling from his work in a multi-pronged initiative with the Documenting COVID-19 project, an online repository of local, state, and federal public records obtained through open-records requests by reporters at the Brown Institute for Media Innovation and collaborative news site Muckrock. Journalists working on the project are using this data and modeling to guide on-the-ground reporting in local counties across the US to uncover the true scope of underreported COVID-19 deaths. They’re chronicling their findings in a series of USA Today articles over the next year.
“Accurate and timely mortality surveillance is critical to pandemic preparedness and response efforts,” says Dr. Stokes, whose team of researchers at BUSPH, the University of Pennsylvania, and the Robert Wood Johnson Foundation, has analyzed mortality data in more than 3,000 US counties. “Without accurate mortality data, it becomes very challenging to devise effective policy responses or to develop fair and equitable responses targeting the most heavily affected communities.”
The first two articles of the USA Today series, published on December 9 and December 22, examine the national data and social and racial inequities tied to excess mortality, including the findings thus far of undercounting in rural counties in Louisiana, Missouri, and Mississippi. Subsequent articles will take deeper dives into these hidden deaths at the local level in other US counties, aiming to understanding why and how these deaths are being excluded from official COVID records in each area.
Documenting COVID-19 is also relying on the knowledge and expertise of local journalists, public health researchers, community organizations, medical examiners, coroners, and the general public at large, and encouraging people to participate in this initiative. The team will soon release a “reporting recipe”—a set of journalists can utilize to support their own local reporting on COVID mortality—as well as an open-access form on the online platform AirTable, where anyone can review or upload, or share their thoughts or story tips about these hidden deaths. Anyone who shares information on the database has the option to do so anonymously. Dozens of reporters have already joined the effort.
“Using the data and modeling that Dr. Stokes’ team has provided, we’re going to continue reporting on undercounted deaths in local areas to explain why these gaps are happening, because the reasons will be different in each area,” says Dillon Bergin, an investigative reporter at Muckrock, and who is part of the Documenting COVID-19 project and reporting team for the USA Today series. “We want to help reporters find their stories, so we’ve also built a core set of tools to help local news groups find the data in their areas and do the investigations they want to do, but may not have the resources to do.”
The fact that so many of these uncounted deaths are occurring at home, and not in a hospital setting where testing is most prevalent, is a factor that warrants further investigation, says Dr. Stokes.
“Much of the underreporting appears to be concentrated among deaths occurring at home, where testing is extremely limited. In these cases, the cause of death is frequently assigned to other conditions such as heart disease or diabetes,” he says. “Many people are afraid of going to the hospital and potentially getting COVID, or losing contact with their loved ones, so they’re getting sick and staying at home, and then dying without their death ever being reported as a COVID death.”
COVID death undercounting also has political implications, says Dr. Stokes. Since most death investigations occur at the county level, the official cause of death is often determined by elected coroners who may be motivated by political bias to downplay the pandemic (and who typically receive less formal training than medical examiners).
Source: Read Full Article
