The latest data on universal screening for type 1 diabetes (T1D) is reviewed in a session at this year’s Annual Meeting of the European Association for the Study of Diabetes (EASD) in Hamburg, Germany (2–6 October). The talk will be given by Dr. Emily K. Sims, Associate Professor of Pediatrics, Center for Diabetes and Metabolic Diseases, Indiana University School of Medicine, Indianapolis, IN, U.S..
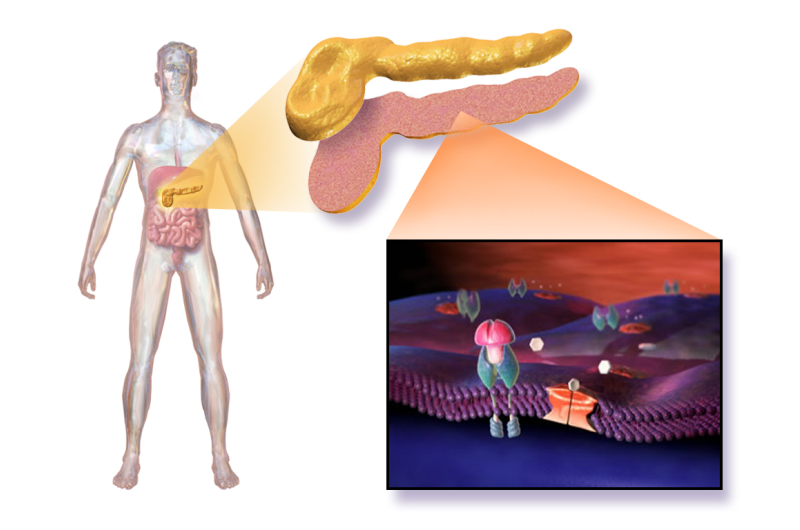
Research by various groups has established that individuals with multiple islet autoantibodies (biomarkers showing that the body is attacking and killing its own insulin producing beta cells in the pancreas) have a near 100% risk of developing T1D over their lifetime, according to a 2013 JAMA study.
Multiple groups including Ezio Bonifacio and colleagues from the TEDDY Consortium, writing in Diabetes Care in 2021, and Ghalwash and colleagues from a Type 1 Diabetes Intelligence Study Group writing in The Lancet Diabetes & Endocrinology in 2022, have shown that screening for islet auto-antibodies at two ages—at age 2 and at 5–7 years—would predict most cases of type 1 diabetes that would develop by age 15 years.
Dr. Sims will highlight that although screening programs have previously most often focused on people with family members with T1D (who can have up to 15 times increased risk of developing T1D), most people who develop T1D (85-90%) have no family history of the condition.
“Our knowledge of type 1 diabetes has now evolved from thinking it is a disease that suddenly develops, to knowing that it is something that gradually develops, after the appearance of multiple islet-autoantibodies. By screening children and adults to identify individuals with early, presymptomatic stages of disease, we can more accurately predict when they will first need insulin and prevent life-threatening DKA episodes that otherwise frequently occur at diagnosis,” she explains. “Natural history studies have shown us that once someone has reached the threshold of multiple islet autoantibodies, progression occurs similarly in relatives and those with no family history.”
Knowing who is likely to develop T1D will help prevent cases of diabetic ketoacidosis (DKA) that occurs when the body doesn’t have enough insulin to allow blood sugar into the cells for use as energy. Instead, the liver breaks down fat for fuel, producing acids called ketones; the build-up of these ketones to dangerous levels causes DKA. These episodes can be dangerous and even fatal, causing a number of uncomfortable symptoms. The symptoms of DKA can be the first sign of T1D in people who haven’t yet been diagnosed.
Various research programs are going on worldwide to establish the best ways of implementing universal screening, including programs in Germany, the U.S., Israel, the UK, and Australia, and a new program (Edent1fi) will include multiple new countries in Europe, including the UK, Germany, Poland, Portugal, Italy and the Czech Republic.
“These are all research programs. The next steps before universal screening for type 1 diabetes becomes general policy will require guidelines for monitoring and endorsement of screening and monitoring guidelines by applicable societies,” explains Dr. Sims. This will also be helped by broader access to disease modifying therapies to impact progression and the need to start insulin injections.
She explains that these research programs are in many cases working with primary care doctors to obtain blood testing for autoantibodies—while some of them work through newborn screening (genetic testing performed on infant blood spots followed by antibody screening in individuals at higher genetic risk).
Dr. Sims says, “The costs of screening, optimal ways to scale it up, and how to connect it with access to disease modifying therapies, such as the monoclonal anti-CD3 antibody that was recently FDA-approved in the US for delay of Stage 3 T1D in individuals meeting criteria for Stage 2 disease (multiple islet autoantibodies and changes in blood sugar), are all still to be worked out. Other important considerations moving forward include reaching traditionally understudied populations and more tailored approaches for individual patients.”
As the question of when we could see universal screening for T1D rolled, Dr. Sims concludes, “I think we will start to see increasing society endorsement of screening and monitoring guidelines over the next five years and that as this occurs, countries will start incorporating screening into routine care for young children at the general practitioner’s office—for example, when children are called for routine childhood vaccinations.”
Screening for adults, who can also develop T1D, is less well studied. Although optimal approaches have yet to be clearly elucidated, this population will also likely benefit from identification of early stage disease and the advantages of education, monitoring, and access to therapy.
“Given that we know that individuals without a family history are the most likely to present with new T1D and that once they reach criteria for early stage disease, they are at similar risk to individuals with a family history, universal screening the of general population is key to ultimately allow the most individuals to benefit from access to education, monitoring, and disease modifying therapies,” says Dr. Sims.
Journal information:
Diabetes Care
,
Journal of the American Medical Association
,
The Lancet Diabetes & Endocrinology
Source: Read Full Article
