A multicenter study led by researchers at Sylvester Comprehensive Cancer Center at the University of Miami Miller School of Medicine shows how interactions between tumor cells and immune components of the microenvironment can impact treatment responses and outcomes in patients newly diagnosed with multiple myeloma who undergo combination treatments that include targeted immunotherapy.
New drugs developed over the past two decades have dramatically improved survival rates, with “deep” and sustained treatment responses associated with low rates of progression. Immunotherapies targeting a molecule, CD38, that is found on multiple myeloma cells have been particularly effective, but even with treatment regimens that include CD38-targeting, the disease fails to respond adequately or progresses prematurely in 30% to 50% of newly diagnosed patients.
“Since the introduction of advanced, targeted immunotherapy regimens, there has been a pressing need to better understand the tumor genomic and immune interactions that drive resistance to combination treatment approaches. This study adds significant information that will result in better clinical trials and more effective therapies for patients with high-risk disease,” said Dr. C. Ola Landgren, hematologist/oncologist, chief of the Division of Myeloma and director of the Myeloma Institute at Sylvester, and co-senior author of an article in Nature Cancer.
Some harmful changes occurring in the genetic makeup of tumor cells are driven by the tumors themselves; others may come about as immunotherapies change the treatment landscape, creating a moving target for researchers and clinicians. Many newly diagnosed patients are treated with therapies affecting the immune microenvironment.
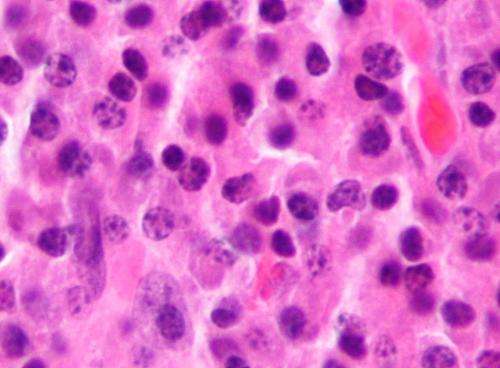
Multiple myeloma, a cancer of plasma cells in the bone marrow, can damage bones and the immune system and often leads to kidney disorders. It affects 35,000 Americans every year, and, at the current time, over 170,000 people are living with multiple myeloma in the United States.
In this study, the researchers collected bone marrow samples from 49 patients who had been treated with combination drug therapy that included a CD38-targeting monoclonal antibody called daratumumab, or DKRd. They employed whole genome sequencing to look for chromosomal changes in tumor cells that could increase risk for treatment resistance, and they used single-cell RNA sequencing to analyze the tumor microenvironment—providing the first in-depth look at the relationship between the two.
“We found that stronger treatment responses and prolonged progression-free survival were driven by a complex interplay between tumor genomic features and immune microenvironment changes,” said Dr. Francesco Maura, a co-first author of the paper whose Sylvester laboratory conducts myeloma computational and translational research.
“Interestingly, we found that with the introduction of immunotherapy, some historically important genomic prognostic factors lost some of their power to predict outcome and a number of genomic drivers and microenvironmental features emerged as being of importance.”
In the article, the researchers identify specific gene mutations and changes that impact clinical outcomes. They also describe immune-related factors and events that predict sustained treatment effects with prolonged survival.
Colleagues from Perlmutter Cancer Center at NYU Langone Health, Memorial Sloan Kettering Cancer Center and Weill Cornell Medical College collaborated on the study with the Sylvester researchers. Dr. Gareth Morgan at Perlmutter Cancer Center is co-senior author of the article. Sylvester’s Dr. David Coffey is a co-first author, as are Dr. Eileen Boyle, of Perlmutter, and Dr. Kylee Maclachlan, of MSK and Weill Cornell.
More information:
Genomic and immune signatures predict clinical outcome in newly diagnosed multiple myeloma treated with immunotherapy regimens, Nature Cancer (2023). DOI: 10.1038/s43018-023-00657-1. www.nature.com/articles/s43018-023-00657-1
Journal information:
Nature Cancer
Source: Read Full Article
