While there are highly effective treatments for the hepatitis C virus (HCV), only one in five Medicaid enrollees diagnosed with HCV started treatment, according to a retrospective study led by researchers at Weill Cornell Medicine and Cornell University’s Ithaca campus.
The findings revealed that treatment uptake rates were even lower among people under 30, women, Hispanic and Asian individuals, as well as people who inject drugs. The research underscores the urgent need for public health and policy efforts to improve initiation and reduce treatment disparities in Medicaid beneficiaries.
“Direct-acting antiviral treatments for hepatitis C infection introduced in the past decade achieved cure rates consistently higher than 90% in clinical trials and are well tolerated,” said lead study author Dr. Shashi Kapadia, M.S. ’17, an assistant professor of medicine in the Division of Infectious Diseases and of population health sciences at Weill Cornell Medicine. “However, we’re nowhere close to reducing the burden of hepatitis C in the United States and are falling well short of the WHO target to eliminate HCV by 2030.”
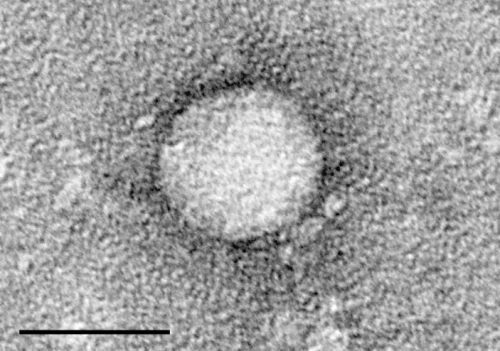
Hepatitis C is a viral infection that causes liver damage and inflammation. It spreads through contact with the blood of an infected person. In the United States, sharing injection drug equipment and having unprotected sex are the most common sources of HCV transmission. It was previously concentrated in the baby boomer generation, but in recent years, infection rates have increased in other groups, including those under 40 and people who inject drugs; 55% of people who inject drugs are Medicaid beneficiaries.
For their study, published Aug. 4 in JAMA Network Open, the investigators examined medication uptake rates within six months of diagnosis for adults ages 18 to 64 using national Medicaid claims from 2017 to 2019. They analyzed disparities by age, sex, race and ethnicity, as well as injection drug use, alcohol use disorder, mental health diagnoses, cirrhosis and HIV infection.
The analysis revealed only 20%—about 18,000 of approximately 87,500 Medicaid enrollees diagnosed with HCV—began treatment within six months. Treatment uptake rates were significantly lower among particular groups: 17% for women compared with 23% for men, 14% for those ages 18 to 29 compared with 24% for those 50 to 64, and 18% for people with a history of injection drug use compared with 23% for those with no history of injection drug use.
Treatment rates were also lower for Asian and Native Americans at 17% and 16%, respectively, compared with 20% for non-Hispanic white people. After adjusting for the influence of other clinical and sociodemographic factors, they also found lower treatment rates among Hispanic individuals compared to non-Hispanic white individuals.
“Our findings highlight the need for targeted outreach programs to ensure more younger people, and particularly those who inject drugs, are tested for hepatitis C and educate both patients and providers that treatment is highly effective and prevents a lot of suffering,” said Kapadia, who is also an attending physician at New York–Presbyterian/Weill Cornell Medical Center.
“We also need more studies to determine the underlying drivers of lower treatment access in some of these groups, such as women and Asian and Native American populations, so that we can tailor interventions to raise their treatment rates.”
More information:
Shashi N. Kapadia et al, Hepatitis C Treatment Initiation Among US Medicaid Enrollees, JAMA Network Open (2023). DOI: 10.1001/jamanetworkopen.2023.27326
Journal information:
JAMA Network Open
Source: Read Full Article
