Murdoch University and Imperial College London researchers have come together to uncover one of the root molecular mechanisms of Alzheimer’s disease.
“We have long known that there are multiple genetic influences on Alzheimer’s risk, but remarkably little is known about how those gene variations actually physically cause the disease,” said Professor Elaine Holmes, ARC Laureate Fellow and Director of the Center for Computational and Systems Medicine.
“This new research links the abnormal genes to blood plasma metabolites—the substances made when the body breaks down food, drugs or chemicals—to detect the most important metabolites impacted by the genetic abnormality.”
Professor Holmes says the discovery, now published in Proceedings of the National Academy of Sciences, lays crucial groundwork for the development of future therapies.
“Once specific biomarker pathways are detected as being abnormal in any disease then we can start to think on which drugs we might use to block or modify for those diseases,” said Professor Holmes.
“So, in this case, we have some new molecular targets for Alzheimer’s that might be useful in halting or slowing down the disease progression.”
It’s important research on a global scale, given that every three seconds someone in the world develops dementia. This poorly understood disease is now the second leading cause of death of Australians. Among women, it’s the leading cause, responsible for 11% of deaths each year.
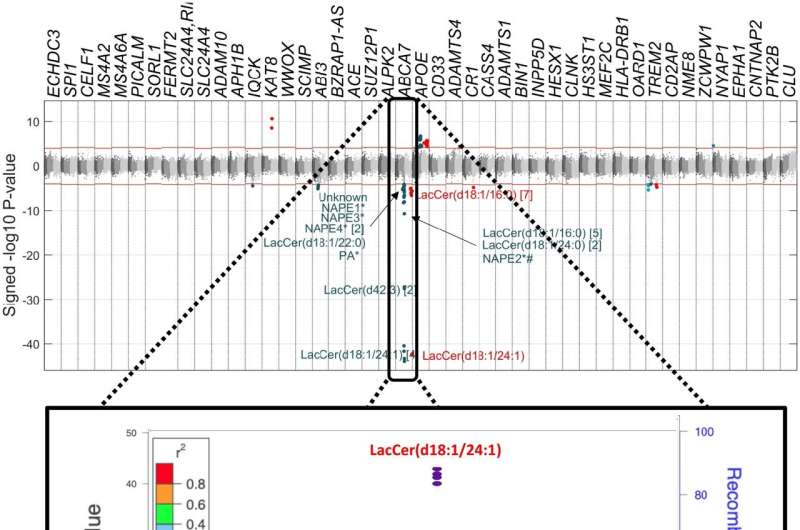
The discovery was made by applying a new analytical technique, Metabolome Wide Association Studies (MWAS), which was originally developed by Professor Holmes and longtime collaborator Professor Jeremy Nicholson, to help understand the metabolites that underpin a person’s risk of disease.
Specifically, Professor Holmes and fellow author Dr. Luke Whiley analyzed the most significant gene variants detected in Alzheimer’s patients and then used statistical analysis to find out how these connected to a large array of blood lipids, or fats, in the body.
Some of these connections turned out to be highly significant, pointing to a new class of metabolites (Lactoceramides) that were genetically-driven.
“The blood levels of Lactoceramides were found to be directly related to patient cognitive performance and longer-term Alzheimer’s risk,” said Dr. Whiley. “This tell is that they are of direct diagnostic and prognostic relevance.”
Dementia occurs when there is a build-up of protein on the brain which causes a slow decline in brain function over the years.
However, while a pathologist knows what to look for, we still don’t have a single confirmed theory as to why those proteins build up and why they cause cognitive decline. Dr. Whiley says this gap in our understanding of the disease’s progression means the development of therapeutics is crucial for patents.
“For diseases of old age, it’s not necessarily about curing or preventing the disease, but if you can delay it by ten or twenty years then you can potentially shift the symptoms beyond a person’s lifetime to improve their quality of life as they get older.”
Professor Nicholson, Pro-Vice Chancellor for Health Sciences at Murdoch said the research exemplifies the type of breakthroughs possible when powerful technologies and effective collaboration come together.
“Western Australia is in a uniquely positioned to help solve some of the world’s most challenging biomedical problems. It is home to the Australian National Phenome Center, the most powerful metabolic phenotyping laboratory of its type in the world,” said Professor Nicholson.
Source: Read Full Article
