Women with a breast cancer diagnosis undergoing procedures for fertility preservation are not at increased risk of recurrence of the disease or disease-specific mortality. This has been shown in a study by Karolinska Institutet in Sweden that followed the participants for five years on average. The results, published in the journal JAMA Oncology, could in the future provide safety and new hope to women who want to preserve their fertility after cancer treatment with chemotherapy.
Almost one in ten women affected by breast cancer are of childbearing age and are at risk of becoming infertile from chemotherapy treatment. With the hope of being able to have children after completing cancer treatment, many women choose to undergo procedures for fertility preservation with or without hormonal stimulation. These methods include cryopreservation, the freezing of embryos, female gametes (oocytes) and ovarian tissue.
“It is not unusual that women with hormone-positive breast cancer or their treating doctors opt out of the procedures for fertility preservation because of the fear that these procedures will increase the risk of cancer recurrence or death. In some cases, women are also advised to wait 5-10 years before trying to conceive, and with increasing age, fecundity in all women decreases. More knowledge is therefore needed about the safety of procedures for fertility preservation at the time of a breast cancer diagnosis,” says the study’s first author Anna Marklund, researcher at the Department of Oncology-Pathology, Karolinska Institutet.
In this study, researchers at Karolinska Institutet and Karolinska University Hospital have investigated whether procedures for fertility preservation in connection with a breast cancer diagnosis entail an increased risk of disease recurrence or death. The study followed the women for five years on average.
The registry study covers 1,275 women of childbearing age who were treated for breast cancer between 1994-2017 in Sweden. Of these, 425 underwent procedures for fertility preservation with or without hormonal stimulation. The control group of 850 women were treated for breast cancer but did not undergo procedures for fertility preservation.
The women who underwent procedures for fertility preservation and the women in the control group were matched on age at diagnosis, calendar period at diagnosis and healthcare region. The statistical data were taken from both nationwide healthcare registers and population registers with data on outcomes, disease- and treatment-related variables and socio-economic characteristics.
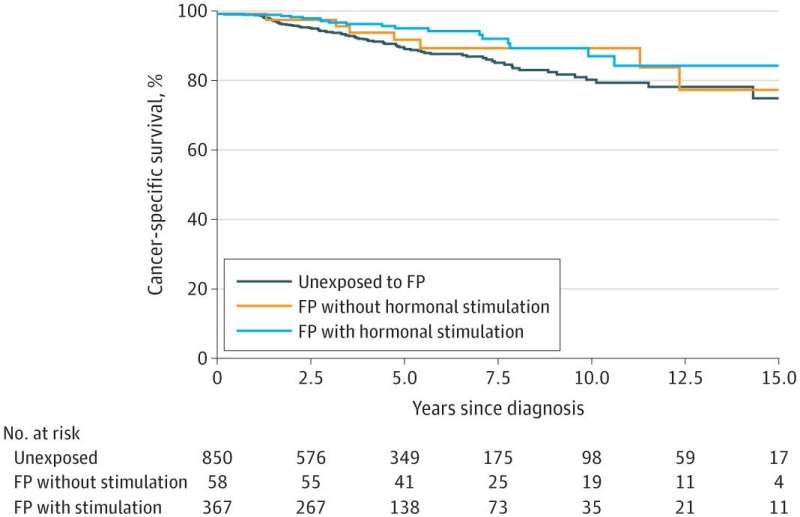
The proportion of women without relapse over the five years was 89 percent among those that underwent hormonal stimulation of the ovaries, 83 percent among women with ovarian tissue freezing, and 82 percent among women who did not undergo procedures for fertility preservation.
Five years after treatment for breast cancer, the survival rate was 96 percent in the group that underwent hormonal stimulation to freeze eggs or embryos, 93 percent in the group that underwent procedures for fertility preservation who did not undergo hormone stimulation and 90 percent in the group that did not undergo procedures for fertility preservation.
“We did not see any increased risk of relapse or mortality when procedures for fertility preservation were undertaken, compared to the women who did not undergo procedures for fertility preservation. This is valuable information that can contribute to changed care routines when it comes to young women with breast cancer who want to preserve their fertility,” says the study’s last author Kenny Rodriguez-Wallberg, adjunct professor and research group leader at the Department of Oncology-Pathology, Karolinska Institutet, and chief physician at Karolinska University Hospital.
Source: Read Full Article
