As scientists, we’re accustomed to reading about our medical research topics in academic publications, such as the British Medical Journal, and not so much via scrolling through sites like Buzzfeed. However, if there is one trendy medical term for 2023, it’s the microbiome. And mainstream stories about probiotics are everywhere. As a culture of wellness continues to gain momentum, we wanted to share our latest research findings and also issue a very important health warning.
At Basel University Hospital of Psychiatry in Switzerland, a multidisciplinary team of psychiatrists and neuroscientists recently published ground-breaking research for the use of probiotics during the clinical management of major depressive disorder (MDD) in the Journal of Affective Disorders. Dr. André Schmidt (Ph.D., PD), one of the authors of this article, led the study from a psychiatric point of view. Professor Claudio De Simone (MD, AGAF), the other author of this article, is a gastroenterologist who developed the formulation (the De Simone Formulation) that Dr. Schmidt’s team used in the study.
The trial added a probiotic formulation into the treatment plan for people experiencing clinical depression to enhance their gut microbiota with the aim to help reduce depressive symptoms.
The results are published in the journal article “Effects of a probiotic add-on treatment on fronto-limbic brain structure, function, and perfusion in depression: Secondary neuroimaging and findings of a randomized controlled trial.”
All participants in the study were prescribed an antidepressant. Half of them received a probiotic add-on. The other half got a placebo. Neither the study participants nor the study staff knew whether the patients were taking probiotics or the placebo. Depressive symptoms were measured with the 17-items Hamilton Depression Rating Scale (HAM-D). Clinical and MRI assessments were conducted before and after the four-weeks intervention.
Clinical data was also assessed at a four-week follow-up after the end of the intervention. Depressive symptoms were measured with the 17-item Hamilton Depression Rating Scale (HAM-D). Clinical and MRI assessments were conducted before and after the four-week intervention. Clinical data was also assessed at a four-week follow-up after the end of the intervention.
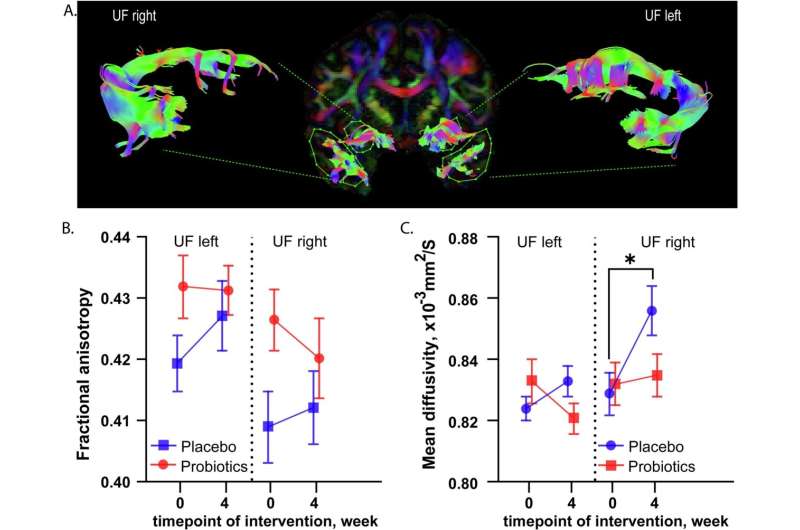
Dr. Schmidt’s researchers found that the people who took the probiotic had signs of preserved structural integrity and fewer signs of neurodegeneration. Furthermore, probiotic supplementation altered the function of fronto-limbic brain regions, a neural circuitry implicated in depression.
Some of the imaging radiology findings were accompanied by improvement in depressive symptoms, prompting the study team to presume that the beneficial clinical effects of probiotic supplementation in depression may be due to a protective effect against neuronal degeneration and alterations in fronto-limbic functioning.
As the inventor of the probiotic formulation used in the study, Professor De Simone explains the science behind why it helped the study participants reduce symptoms and improve overall health. In this study, the microbiome’s enhancement is linked not just to the specific bacteria strains used, but the unique biochemical and immunological enzymatic profile that results from the formulation’s method of production and blending.
Professor De Simone explains that the clinical results obtained with any individual formulation are specific and “not exportable” to other products due to different and proprietary production methods, even if the strains might be genetically equivalent. In simple terms, using any probiotic product without matching it to the condition first might not achieve the desired results, and could even cause harm in vulnerable patient groups.
As a guideline for using probiotics during the clinical management of conditions, the U.S. headquartered International Scientific Association for Probiotics and Prebiotics (ISAPP) recently published their recommendations to support the scientific and medical community on judging probiotic safety. In the article titled “Emerging issues in probiotic safety: 2023 perspectives,” published in the journal of Gut Microbes, the authors make it clear that probiotics are generally safe in healthy people, but adverse events can and do occasionally occur in vulnerable groups.
Research shows that quality probiotics are generally safe in healthy people, but adverse events can and do occasionally occur in vulnerable groups.
As for limitations to the study, Dr. Schmidt says an additional follow-up MRI session would be interesting for seeing clearer changes in the relevant brain regions as clinical effects were strongest in follow-up. The Basel team believes this is an important area of research that requires more attention with additional studies that can offer pathways to healing. As clinicians we believe in the importance of recognizing mental health is an essential part of a person’s overall health and well-being, and that mental conditions are common and treatable.
This story is part of Science X Dialog, where researchers can report findings from their published research articles. Visit this page for information about ScienceX Dialog and how to participate.
More information:
Gulnara Yamanbaeva et al, Effects of a probiotic add-on treatment on fronto-limbic brain structure, function, and perfusion in depression: Secondary neuroimaging findings of a randomized controlled trial, Journal of Affective Disorders (2023). DOI: 10.1016/j.jad.2022.12.142.
Daniel Merenstein et al, Emerging issues in probiotic safety: 2023 perspectives, Gut Microbes (2023). DOI: 10.1080/19490976.2023.2185034
Dr. Schmidt Bio:
Dr. André Schmidt (PhD, PD) is psychiatric neuroscientist with a particular interest in clinical neuroimaging, cognitive neuroscience and psychopharmacology. The main focus of his work is designing and conducting basic and clinical research with a specific focus on neuropsychopharmacology, neuroimaging and clinical neuroscience. His research aims to establish reliable biomarkers for clinical services to predict individual disease stages of brain disorders, monitor treatment responses and develop novel interventions. Dr. Schmidt has been the Group leader, Translational Neurosciences, Department of Psychiatry (UPK), University of Basel, Switzerland since 2016.
Professor De Simone Bio:
Professor Claudio De Simone (MD, AGAF) is an internationally recognized European academic in the field of probiotics and the human microbiota. Professor De Simone is a Fellow of the American College of Gastroenterology. He is also a retired professor of infectious diseases at the University of L’Aquila (Italy), where he specialized in gastroenterology, allergology and clinical immunology. Since commercializing his signature De Simone Formulation in the 1990s, the Professor has actively campaigned for better regulation and quality control of probiotics based on potential risks to health and well-being. He has authored more than 200 published case studies, scientific articles and book chapters.
Journal information:
Journal of Affective Disorders
,
British Medical Journal (BMJ)
Source: Read Full Article
