Researchers at Karolinska Institutet and the University of Gothenburg have found another piece of the puzzle in the treatment of the childhood cancer neuroblastoma. A new case report, published in JCO Precision Oncology, describes the successful targeted treatment of a boy with neuroblastoma and a specific mutation.
“Combining genetic mapping and biological understanding with a new targeted treatment is precision medicine made real, which can make a difference and cure more children who have cancer,” says the study’s corresponding author Per Kogner, professor at Karolinska Institutet and pediatric oncologist at Astrid Lindgren Children’s Hospital at Karolinska University Hospital.
A new mutation
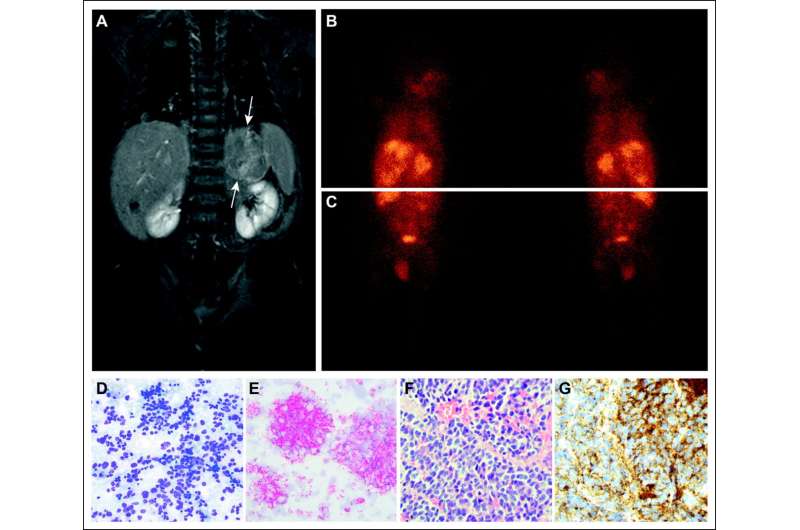
The study is a case report of a little boy who came to the hospital at 6 months of age with a widespread cancer, neuroblastoma. The effects of his cancer were significant and repeated chemotherapy treatments did not provide the improvement hoped for. After an operation where the primary tumor was removed, new genetic analyses could be undertaken, including whole-genome sequencing (analysis of the entire genome) and tumor protein analyses, says one of the study’s first authors, Diana Treis, pediatrician and doctoral student in Per Kogner’s research group at Karolinska Institutet.
Analyses at the University of Gothenburg by Professors Ruth Palmer and Bengt Hallberg showed that two known proteins in cancer cells’ signaling pathways were activated—the so-called ALK and TRKA proteins. Upon closer examination of the gene sequence, no mutation was found in the ALK sequence. Instead, the researchers found that a mutation in the protein that binds to and activates ALK, the ALKAL2 ligand, may have contributed to the onset of neuroblastoma.
Rapid recovery
Shortly before the boy turned two years of age, he was able to start a new targeted treatment with the drug entrectinib, which targets ALK and TRKA. After treatment had started, the boy quickly felt better.
“This is the first case in the world, with this type of cancer and this biology, receiving this particular targeted treatment,” says Per Kogner.
After five years of treatment, the tumor has shrunk so that it is almost completely gone. Per Kogner and his colleagues will continue to monitor the boy to see if and when treatment can be stopped.
Can be important for other children
The development of genetic diagnostic tools and how they are used clinically has progressed rapidly in recent years.
“Today, the whole-genome sequencing of a child who gets neuroblastoma would basically be done on day one of an investigation,” says Tommy Martinsson, professor at the University of Gothenburg and co-author of the study.
Now all children with cancer, about 350 children each year, are offered whole genome sequencing at the time of their diagnosis via a national pilot project in Genomic Medicine Sweden, GMS, a national approach that is unique from an international perspective.
“In addition to providing new treatment options for these children, the pilot study will also show the benefits and how whole genome sequencing could be introduced into healthcare for other cancers as well,” says Tommy Martinsson.
Tailored for each individual patient
Precision medicine is a medical model that is tailored to every individual patient being treated. Advanced methods of examining the genome provide very valuable information. There must also be pharmaceutical substances, clinical studies to study new targeted treatments and the knowledge within molecular biology of signaling pathways.
Source: Read Full Article
