An international consortium of leading experts is calling for governments and health systems to acknowledge that male infertility is a common and serious medical condition that may be increasing worldwide, and has provided a first-time roadmap for urgent, global action.
The consortium is led by the University of Melbourne’s dean of science; among its U.K. representatives is professor Allan Pacey from The University of Manchester.
The scientists from 10 countries compiled a consensus report with 10 recommendations, published in Nature Reviews Urology, which comes as the World Health Organization estimates that infertility now affects one in six couples of reproductive age, in Australia and globally. About half the time, infertility originates from the male.
The report highlights that patients have a right to meaningful diagnoses and targeted treatments, but these are currently unavailable in most cases due to inadequate funding, research gaps, and non-standard clinical practices.
The report recommendations include:
- A global “biobank” of tissues and clinical data from men, and their partners and children to help researchers understand genetic and environmental causes of infertility.
- Genomic sequencing and better diagnostic tests routinely offered to men to help them understand why they are having difficulties fathering a child.
- Rigorous tests of the impacts on men and boys of compounds such as endocrine-disrupting chemicals in everyday consumer products, the workplace, and the general environment.
- Regulations and policies to protect men and boys from disruptive compounds, and development of safe alternatives.
- Better training to help health care workers promote male reproductive health across the lifespan.
Lead author Professor Moira O’Bryan, Dean of Science at the University of Melbourne, said evidence was mounting in Australia and worldwide that male reproductive health has declined over recent decades, but further research was needed.
“Urgent, worldwide action to implement our recommendations is critical,” said Professor O’Bryan, who directs a multidisciplinary program of research and clinical studies in male infertility and male-based contraception.
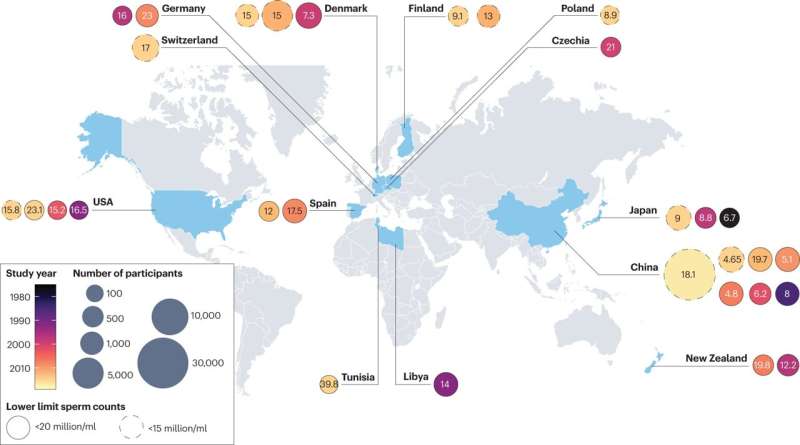
“Decreasing semen quality and increasing frequency of testicular cancer and congenital defects in the urogenital system indicate that, globally, male reproductive health has declined over recent decades. Research is needed to understand why, and how this trend can be reversed.”
Co-author Professor Allan Pacey from the University of Manchester said, “For far too long, the science and medicine which deals with male reproductive health has been in the shadows. If we are truly to understand the risks to male reproductive health, and know how to deal with them, we need a major step change in how this happens. In this paper our working group has proposed its top 10 recommendations which it hopes can help kick-start research and education in male reproductive health around the globe.”
The Male Reproductive Health Initiative—a working group of the European Society for Human Reproduction and Embryology—commissioned 26 experts from Australia, Argentina, Canada, China, Denmark, Germany, Italy, Spain, the United Kingdom, and the United States to produce the evidence-based roadmap that identifies key knowledge gaps, barriers, and opportunities for researchers, governments, health care systems, and public education.
Professor O’Bryan said the report also highlights that men and their partners deserve more support.
“By the time they seek medical advice, men experiencing infertility are often in emotional distress, which is made worse when their doctor can’t determine the cause nor offer any treatment,” she said.
“For most infertile men, the cause of their infertility is unknown. When it is known, few targeted treatments exist. Globally, the huge economic and social burdens of male infertility are not well appreciated. The cost of treatments and the impacts of infertility on mental health, relationships, and productivity are enormous.”
Men are currently designated ‘infertile’ based on family history, physical examination, hormone profiles and semen analyses.
“Unlike many other medical conditions, genetic screening to diagnose male infertility is extremely limited because it is not covered by public health care or insurance, and because research into genetic causes of male infertility has not been funded,” said Professor O’Bryan.
“Given compelling evidence that male infertility can be a biomarker for other diseases, this seems a missed opportunity to improve men’s health on multiple levels.”
The paper’s 26 authors are world leaders in andrology, gynecology, urology, cellular biology, endocrinology, environmental hazards, pathology, reproductive medicine, medically assisted reproduction, oncology, genetics, pediatrics, pharmacology, and therapeutics.
The 10 recommendations:
- Governments, health care systems, insurance companies, and the public should understand and acknowledge that male infertility is a common, serious medical condition and patients have a right to meaningful diagnoses and targeted treatments.
- Establish a global network of registries and biobanks containing standardized clinical and lifestyle information, and tissue from fertile and infertile men, their partners, and children. Link it to national health care data systems.
- Implement protocols and incentives to standardize collection of de-identified tissue and clinical/lifestyle data.
- Fund more international, collaborative research to understand the interactions and impacts of genetic, lifestyle, and environmental factors on male fertility in diverse populations.
- Integrate genomic sequencing into diagnosis of male infertility.
- Develop additional diagnostic tests to improve diagnosis and cause of male infertility.
- Rigorously test the impact on male fertility of compounds—especially endocrine-disrupting chemicals—in products, the workplace, and the environment. Implement regulations and policies and develop safe alternatives.
- Rigorously test strategies for medically assisted reproduction before they are integrated into clinical practice.
- Public education campaigns to promote discussion of male infertility and engagement in health seeking.
- Improved training for health care workers to promote male reproductive health across the lifespan.
More information:
Sarah Kimmins et al, Frequency, morbidity and equity—the case for increased research on male fertility, Nature Reviews Urology (2023). DOI: 10.1038/s41585-023-00820-4
Journal information:
Nature Reviews Urology
Source: Read Full Article
