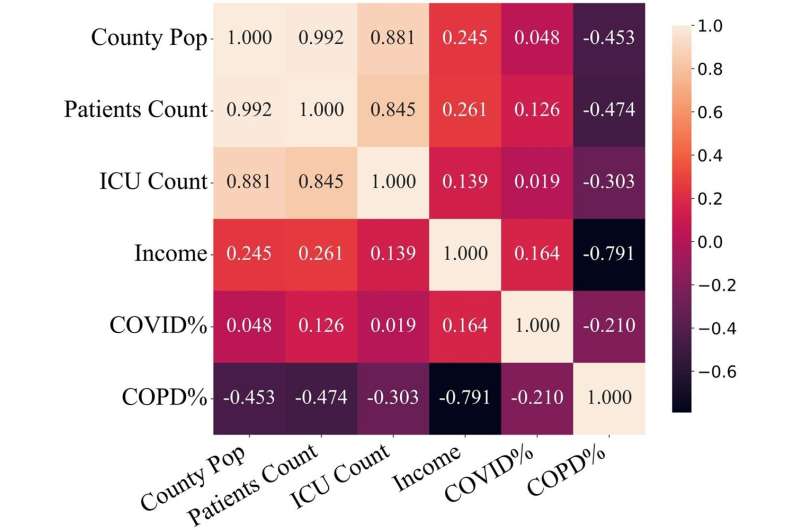
A study of more than three-quarters of a million Indiana COVID-19 cases is one of the first to focus on the disease in the Midwest. The research examines the relationship between the presence of pre-existing disease and COVID-19 outcomes in a region that has some of the highest prevalence of comorbidities, including hypertension, chronic obstructive pulmonary disease (COPD) and diabetes.
The study, conducted by researchers from Regenstrief Institute, Indiana University and The Ohio State University sourced data through the COVID-19 Research Data Commons. For COVID-19 patients, research demonstrated the pre-existing presence of one or more diseases, called comorbidities, was linked to an increased risk of admission to an intensive care unit (ICU) as well as greater likelihood of death.
For many pre-existing conditions, older age, male sex or both augmented risk of ICU admission for COVID patients. Health disparities due to race and to access to healthcare were also found to influence outcomes.
The COVID-19 Research Data Commons was developed by Regenstrief Institute informaticians early in the pandemic and contains information obtained from the Indiana Department of Health and the Indiana Network for Patient Care (INPC). Created by Regenstrief Institute and managed by the Indiana Health Information Exchange, the INPC is one of the nation’s largest clinical data repositories.
“Our examination of this trove of data from throughout Indiana confirms that COVID-19 health disparities—racial, geographic and economic—clearly exist,” said study co-author Regenstrief Institute Research Scientist Titus Schleyer, DMD, Ph.D. “Black patients were much more likely to be admitted to the intensive care unit (ICU) with COVID-19 than White patients, indicating that Black patients had more severe cases of the disease than White patients. Disparities were also found between rural and urban areas.”
“Our work validates findings from smaller and less geographically comprehensive studies and also helps resolve previous conflicting findings. This is one of the biggest studies looking at how pre-existing disease influences the COVID experience and it allows us to better predict who is going to get infected by COVID—and potentially similar viruses—and suffer more.”
“We analyzed COVID-19 positive patients as well as healthy and nonhealthy patients who did not have COVID as controls for the datasets,” said study corresponding author Xia Ning, Ph.D., a Regenstrief Institute affiliated scientist and faculty member at The Ohio State University. “The large amount of robust electronic health record data from the COVID-19 Research Data Commons provided a relatively complete picture of COVID throughout Indiana from the critical, initial period of the pandemic before home test kits became available.”
“The question of why we are interested in researching COVID, now that it’s almost ‘conquered’, is an important one,” noted Dr. Schleyer. “The answer is simple—the next infection is really just right around the corner. It’s not a question of if a pandemic like COVID will happen, but when. There are many pathogens—bacterial or viral—that could have the same or similar infection rates as COVID.”
“There are hypotheses that COVID was caused by people getting infected by interaction with wild animals, and that’s clearly a risk as more humans have more contact with wild animals. There’s another risk that most people don’t know about, which is that climate change is thawing permafrost. Permafrost has kept potentially dangerous pathogens locked up for thousands and thousands of years.”
“With the thawing of permafrost, those pathogens have an opportunity to get into the air; get into the flora and fauna, and, obviously, eventually could be transmitted to humans. It’s very important that we don’t just wash our hands of COVID. Rather, we need continue to learn lessons to prevent or at least mitigate the next pandemic that’s going to surely come.”
The paper is published in the journal JAMIA Open.
More information:
Nader Zidan et al, Understanding comorbidities and health disparities related to COVID-19: a comprehensive study of 776 936 cases and 1 362 545 controls in the state of Indiana, USA, JAMIA Open (2023). DOI: 10.1093/jamiaopen/ooad002
Journal information:
JAMIA Open
Source: Read Full Article
