In a world first, scientists at Duke-NUS Medical School, the National Heart Center Singapore (NHCS) and colleagues in Germany have shown that regenerative therapy to restore impaired kidney function may soon be a possibility.
In a preclinical study reported in Nature Communications, the team found that blocking a damaging and scar-regulating protein called interleukin-11 (IL-11) enables damaged kidney cells to regenerate, restoring impaired kidney function due to disease and acute injuries.
“Kidney failure is a global epidemic,” said Assistant Professor Anissa Widjaja, a molecular biologist with Duke-NUS’ Cardiovascular & Metabolic Disorders (CVMD) Signature Research Program. “Closer to home, Singapore ranks first in the world for diabetes-induced kidney failure and fourth in terms of kidney failure prevalence. The contribution of chronic kidney disease to mortality is rapidly increasing, suggesting there are shortcomings in current therapeutic approaches.”
Searching for ways to restore the kidney’s ability to regenerate damaged cells, Widjaja worked with Professor Stuart Cook, Tanoto Foundation Professor of Cardiovascular Medicine at the SingHealth Duke-NUS Academic Medical Center and the CVMD Program, and Clinician Scientist and Senior Consultant with the Department of Cardiology, NHCS, and Duke-NUS Dean Professor Thomas Coffman, a world-leading nephrologist. They teamed up with scientists in Germany to investigate the role of IL-11, which is known to trigger scarring in other organs, including the liver, lungs and heart, in acute and chronic kidney disease.
Their findings implicate the protein in triggering a cascade of molecular processes in response to kidney injury that leads to inflammation, fibrosis (scarring) and loss of function. They also discovered that inhibiting IL-11 with a neutralizing antibody can prevent and even reverse kidney damage in this setting.
“We found that IL-11 is detrimental to kidney function and triggers the development of chronic kidney disease,” said Cook. “We also showed that anti-IL11 therapy can treat kidney failure, reverse established chronic kidney disease, and restore kidney function by promoting regeneration in mice, while being safe for long term use.”
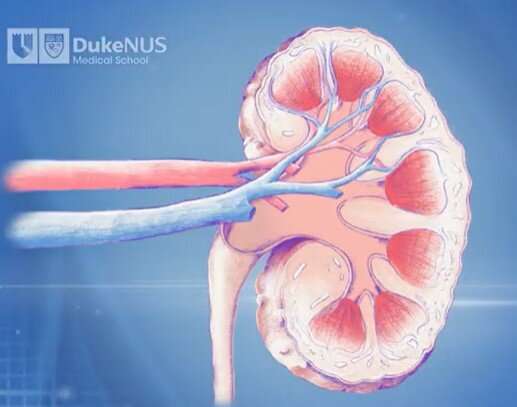
More specifically, the researchers showed that renal tubular cells, which line the tiny tubes inside kidneys, release IL-11 in response to kidney damage. This turns on a signaling cascade that ultimately leads to increased expression of a gene, called Snail Family Transcriptional Repressor 1 (SNAI1), which arrests cellular growth and promotes kidney dysfunction.
In a preclinical model of human diabetic kidney disease, turning off this process by administering an antibody that binds to IL-11 led to proliferation of the kidney tubule cells and reversal of fibrosis and inflammation, resulting in the regeneration of the injured kidney and the restoration of renal function.
While clinical trials of an antibody that binds to another pro-fibrotic molecule called transforming growth factor beta have been unsuccessful, this new approach brings hope of a new target.
“By boosting the kidney’s intrinsic capability to regenerate, Prof. Cook and Asst. Prof. Widjaja have shown that we can restore function to a damaged kidney,” said Coffman, who is also the principal investigator of the Diabetes Study in Nephropathy and other Microvascular Complications (DYNAMO), a large collaborative study that aims to find new solutions for the prevention and treatment of diabetic kidney disease.
“This discovery could be a real game-changer in the treatment of chronic kidney disease—which is a major public health concern in Singapore and globally—bringing us one step closer to delivering the benefits promised by regenerative medicine.”
More information:
Anissa A. Widjaja et al, Targeting endogenous kidney regeneration using anti-IL11 therapy in acute and chronic models of kidney disease, Nature Communications (2022). DOI: 10.1038/s41467-022-35306-1
Journal information:
Nature Communications
Source: Read Full Article
