Fungal infections cause 1.5M+ deaths each year, and there’s no vaccine to prevent them
A new vaccine from the University of Georgia could be the first clinically approved immunization to protect against invasive fungal infections, a growing concern as antifungal drug resistance increases.
Fungal infections cause more than 1.5 million deaths worldwide each year and cost billions. They also double hospitalization costs, double the length of hospital stays and double the risk of death in hospitalized patients, according to a previous UGA study.
But there currently are no effective vaccines to protect vulnerable patients from fungal infections.
“There’s a significant unmet clinical need for this kind of prevention and also treatment, particularly among immunocompromised individuals,” said Karen Norris, lead investigator on the new study published in PNAS Nexus and professor in the College of Veterinary Medicine. “The patient population at risk for invasive fungal infections has increased significantly over the last several years.”
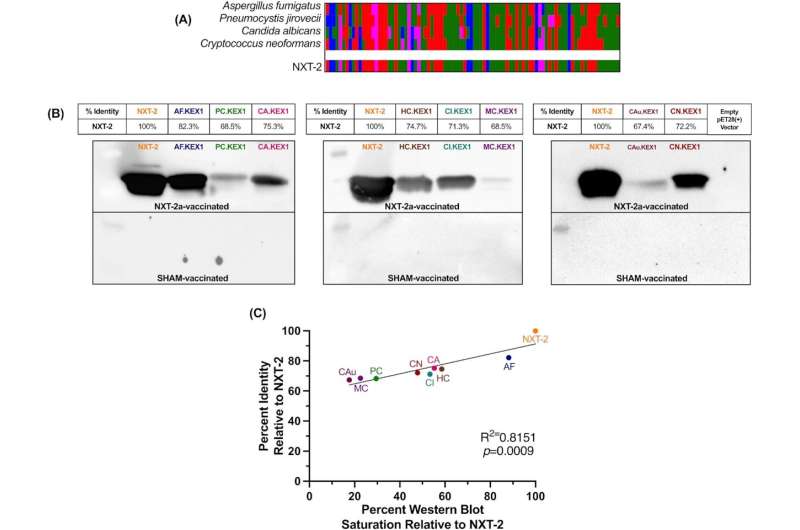
The experimental vaccine is designed to protect against the three most common fungal pathogens that are responsible for more than 80% of fatal fungal infections. The study tested the vaccine’s efficacy in four preclinical animal models, including nonhuman primates.
The researchers relied on different immunosuppressed models for the study, reflecting drug regimens similar to those of transplant recipients, people with HIV or cancer patients, some of the most at-risk human populations.
The vaccine was effective in developing protective antibodies in each of the models.
“Because it targets three different pathogens, the vaccine has the potential to be groundbreaking regarding invasive fungal infections,” said Norris, who is also faculty in the university’s Center for Vaccines and Immunology. “Plans are underway to develop the vaccine for a Phase I (human) safety trial.”
More people at risk of fungal infections than just immunocompromised
Fungal infections are most commonly seen in people with immune disorders, including those with uncontrolled HIV or impaired immunity from therapies like chemotherapy or anti-inflammatories.
But previous research from Norris, postdoctoral fellow Emily Rayens and the College of Public Health’s José Cordero in 2022 showed that at-risk population has expanded in recent years.
That study showed people with diabetes; chronic obstructive pulmonary disease (or COPD); or co-infections such as COVID-19, tuberculosis or flu are likewise at higher risk of developing fungal infections.
The first line of defense is typically treatment with azoles, which are broad-spectrum anti-fungal medications. But antifungal resistance is growing. As a result, fungal infections are becoming more difficult to treat, making prevention even more critical, Norris said.
The new vaccine targets the three most common causes of fungal infections: Aspergillus, Candida and Pneumocystis. Candida, in particular, is a growing concern in health care circles as different strains of the fungus become multidrug resistant.
The vaccine showed broad, cross-protective antifungal immunity in the animal models, which bodes well for future clinical trials.
“This is an area that has been underdeveloped on the research front for a long time,” said Norris, who is also the Georgia Research Alliance Eminent Scholar in Immunology and Translational Biomedicine. “These are very large populations of people who are at risk of invasive fungal infections, and although there has been considerable efforts to develop vaccines, none are yet approved. We believe this is a very strong vaccine candidate.”
More information:
Emily Rayens et al, Immunogenicity and protective efficacy of a pan-fungal vaccine in preclinical models of aspergillosis, candidiasis, and pneumocystosis, PNAS Nexus (2022). DOI: 10.1093/pnasnexus/pgac248
Journal information:
PNAS Nexus
Source: Read Full Article
