Patients with congenital heart diseases often suffer from obstructions in the right ventricular outflow tract (RVOT), which carries blood from the heart to the lungs. These obstructions can be repaired with surgical procedures. However, these are temporary fixes that can still result in pulmonary stenosis and/or regurgitation, eventually leading to RVOT dysfunction and even fatal arrhythmias.
Often, heart patients require pulmonary valve replacement (PVR) surgery; using bioprosthetic valves made from materials derived from cows or pigs, which deteriorate over time. This results in patients needing valve replacement surgeries throughout their lives, which increases the risk of surgical complications.
To minimize the need for multiple surgeries and their resultant risks, medical researchers have been trying to find robust alternatives to surgical PVR. To this end, transcatheter PVR (TPVR) has emerged as a potential non-surgical option to restore RVOT and pulmonary valve functions without the concomitant surgical risks.
In a review article, Professor Adolphus Kai-Tung Chau from the Chinese University of Hong Kong Medical Center discusses the benefits, challenges, clinical considerations, outcomes, and developments in the application of TPVR. The article was made available online on December 5, 2022, in Pediatric Investigation.
“Different cardiology societies may adopt slightly different criteria for TPVR for both symptomatic and asymptomatic patients. But given that this procedure is minimally invasive compared to surgical PVR, it is likely that more asymptomatic patients may benefit from it,” says Prof. Chau.
The TPVR procedure requires a thorough pre-procedural evaluation, including patient history, physical examination, chest radiographs, electro- and echo-cardiograms, and imaging tests to ascertain the morphology of the RVOT and the presence of existing pulmonary complications. The surgical plan for individual patients is ideally determined by a multidisciplinary team of specialists.
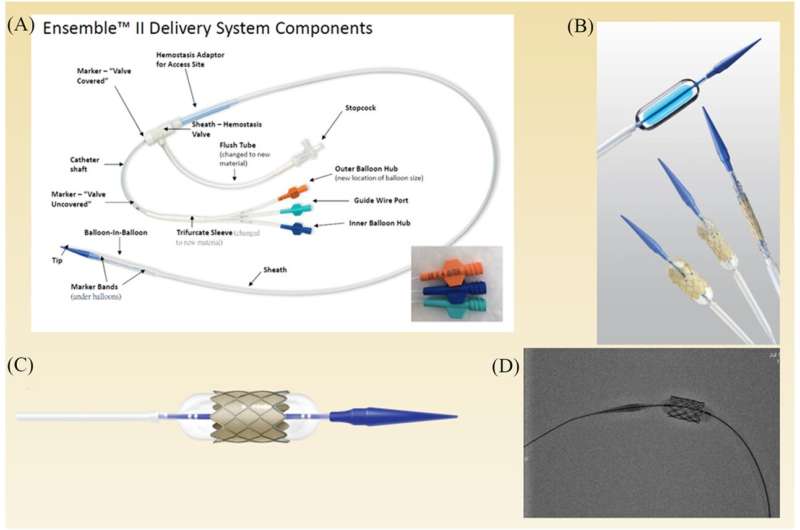
Before the procedure, anatomical and hemodynamic data are assessed along with the assessment of the coronary artery and aorta. Next, the RVOT conduit is prepared for the implantation with pre-stenting and serial balloon dilation to ensure adequate pressure in the right ventricle and avoid valve failure.
What makes the TPVR procedure minimally invasive? Unlike conventional open-heart surgery, TPVR is conducted by guiding a hollow transcatheter tube through the femoral or jugular vein into the heart. The valve is implanted and set in position via balloon dilation. Following the implant, post-procedure hemodynamic data and angiograms are obtained to assess valve competence and check for perivalvular leak.
An advantage of the TPVR is that it can also be safely used for valve-in-valve conditions, where a new transcatheter valve is placed inside the hole of the failed valve after minor alterations.
Lately, trials are being conducted to adapt the application of TPVR for valve implantation in native, large, or variably shaped RVOTs, through self-expanding, partially covered stents that can fit into a wide range of RVOT shapes and sizes.
As of now, the Harmony and Edward Sapien valves are the only TPVR-compatible valves approved by the United States Food and Drug Administration (FDA). However, newer valves are continuously being developed and tested with promising results.
Long-term results indicate that TPVR can effectively restore RVOT function, while improving survival rates and reducing the need for reintervention across age groups. Nevertheless, vigilant testing is recommended to avoid endocarditis and coronary artery compression, which are rare but serious complications of TPVR. Although TPVR and surgical PVR have similar outcomes in terms of mortality rates and cardiovascular readmissions, TPVR leads to shorter hospital stays that benefit both patients and their caregivers.
Source: Read Full Article
