Monkeypox virus can be shed into the surrounding environment by people who are infected, particularly in shed skin particles and in debris from monkeypox skin lesions and scabs. The virus is relatively hardy and under appropriate conditions can remain infectious on surfaces for weeks, creating a potential infection risk to others.
The UK Health Security Agency (UKHSA) recommends that patients with monkeypox who have severe disease requiring hospital admission are cared for in isolation rooms, with infection prevention and control (IPC) precautions that aim to contain potentially infectious virus within the room and protect staff who enter. However, to date it has been unclear whether these measures are proportionate to the potential virus exposure risks.
To investigate this, researchers from the Liverpool School of Tropical Medicine, the University of Oxford’s Nuffield Department of Medicine and the UKHSA conducted a study which collected samples from the rooms of patients hospitalized with monkeypox. The findings have been published in The Lancet Microbe.
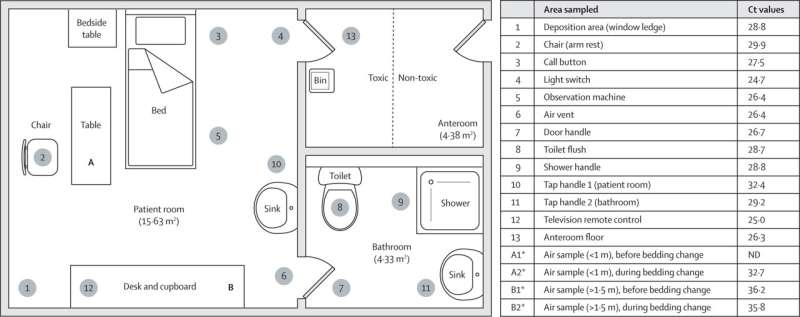
The research team assessed the extent of virus shedding onto surfaces in specialist isolation rooms containing patients admitted to hospital for the management of severe monkeypox. They also investigated whether the virus was detectable in air samples from the rooms.
The researchers found that viral DNA shed by the patients could be found on multiple surfaces throughout the isolation rooms (56 (93%) positive by PCR out of 60 samples). Monkeypox virus DNA was also found on personal protective equipment (PPE) worn by healthcare workers caring for these patients, and in the anterooms where they remove their PPE. Monkeypox virus DNA was also detected in five out of twenty air samples taken within these isolation rooms.
Changing bed linen was an activity particularly associated with detection of monkeypox virus DNA in air samples in the room. This suggests that viral particles, probably in shed skin particles, can become suspended in the air when bed sheets are changed. Monkeypox virus capable of replicating in cells under laboratory conditions (an indicator that the virus could infect other people) was identified in two of four PCR-positive samples selected for virus isolation. This includes air samples collected during the bed linen change.
Lead author, Dr. Susan Gould, from the Liverpool School of Tropical Medicine, says, “Our results found that changing a patient’s bedding appears to be particularly associated with an increased ability to detect monkeypox virus in air samples. In 2018, a UK healthcare worker was thought to have developed monkeypox after being exposed to the virus while changing a patient’s bedding, before monkeypox had been considered and diagnosed. Our results suggest that changing bed linen used by hospitalized patients with monkeypox does indeed increase the risk of exposure to virus, by disturbing virus on bed linen and allowing it to be suspended in the air.”
In addition to detecting virus DNA, the researchers were able to isolate replication-competent virus in some surface and air samples. The results show, for the first time, that monkeypox virus in some air samples taken around patients hospitalized with monkeypox is capable of replicating in cells and is not just ‘dead’ virus. Dr. Gould says that “these results suggest that monkeypox virus shed into a hospitalized patient’s environment poses an infection risk that needs to be managed.”
Senior author on the paper, Dr. Jake Dunning, of the University of Oxford’s Nuffield Department of Medicine and the Royal Free London NHS Foundation Trust, says that “it is important to note that detection of virus, even when demonstrated to be infectious, does not necessarily mean that exposure to the virus in real life would result in infection of the exposed person. However, it does reveal a potential transmission risk and one that is reasonable to control in hospital settings. Our results confirm that the strict IPC measures we follow in specialist infectious diseases centers are necessary and appropriate.”
This investigation specifically evaluated exposure risks when caring for patients admitted to specialist facilities in hospitals. The results and recommendations may therefore not apply to other settings, such as outpatient clinics where patients attend for a short time, interactions differ, and the virus is unlikely to accumulate to such an extent. There is no suggestion that transmission of monkeypox virus via aerosols is a common way for the infection to spread from one person to another.
Dr. Gould added that “in the context of ward-based care, our results support infection prevention and control measures designed to protect against exposure to infectious virus on surfaces and in the air, such as appropriate PPE, as well as applying measures designed to contain shed virus within hospitalized patients’ isolation rooms, including the use of negative pressure rooms and doffing areas.”
The study was led by scientists from the Liverpool School of Tropical Medicine and the University of Oxford, as part of the National Institute for Health and Care Research Health Protection Unit in Emerging and Zoonotic Infections, which includes the University of Liverpool as a partner.
The HPRU in Emerging and Zoonotic Infections and UKHSA identified a need for environmental sampling in hospitals managing inpatients with monkeypox and rapidly began investigations. Prior to publication the team shared its results with those caring for patients with monkeypox admitted to hospitals in the UK, and with international partners, infectious diseases specialist networks, and public health organizations.
Source: Read Full Article
