New research from The University of Texas MD Anderson Cancer Center found that treatment with antihistamines, a commonly used allergy medication, was associated with improved responses to immune checkpoint inhibitors. The preclinical study demonstrated that the histamine receptor H1 (HRH1) acts in tumor-associated macrophages (TAMs) to suppress T cell activation in the tumor microenvironment. The findings were published today in Cancer Cell.
If replicated in prospective clinical trials, the data suggest that targeting HRH1 may be useful as a treatment approach in combination with checkpoint blockade to overcome immunotherapy resistance and improve outcomes, particularly for patients with pre-existing allergies or high plasma histamine levels.
“In searching for factors that might influence responses to immunotherapy, we were surprised to discover that antihistamines, a mediator of the allergy response, were associated with significantly improved outcomes in patients,” said study co-lead Yi Xiao, Ph.D., instructor of Molecular & Cellular Oncology. “Looking closer at this relationship, we discovered that histamine, through its receptor HRH1, can promote cancer cell immune evasion and resistance to immunotherapy.”
Antihistamines associated with improved immunotherapy outcomes
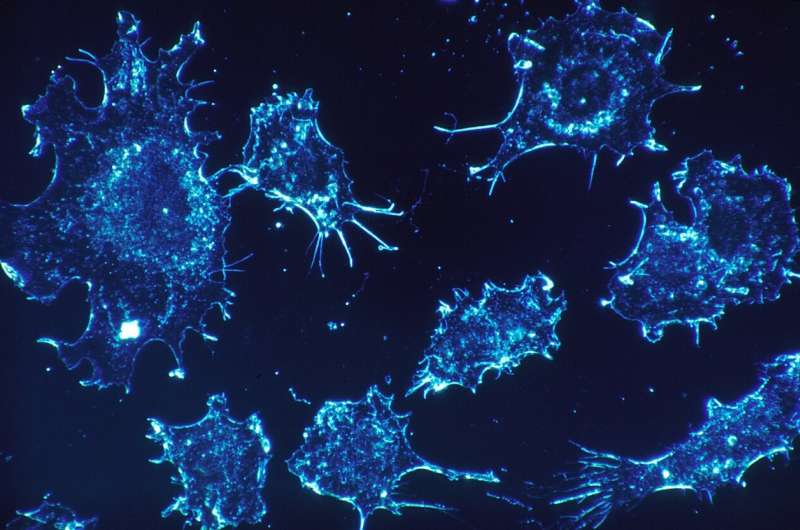
Immune checkpoint inhibitors, a type of immunotherapy, work by blocking certain checkpoint proteins that regulate the activity of T cells, unleashing the T cells to mount an anti-tumor response and eliminate cancer cells. Checkpoint blockade provides long-lasting responses for many patients, but not all benefit equally. Therefore, there is a desire to better understand factors that contribute to immunotherapy sensitivity or resistance.
This study began with the researchers investigating if other commonly used medications might influence responses to checkpoint inhibitors. They performed a retrospective analysis of clinical data from MD Anderson patients undergoing treatment with immune checkpoint inhibitors.
In those with melanoma or lung cancer, concurrent use of antihistamines targeting HRH1 was correlated with significantly improved survival outcomes. Patients with breast or colon cancer also displayed similar trends, although the data did not reach statistical significance due to a relatively small sample size.
Using The Cancer Genome Atlas and other publicly available patient cancer data, the team also discovered that high expression of HRH1 in tumors was correlated with markers of T cell dysfunction, poor responses to checkpoint inhibitors and poorer survival outcomes.
Histamine receptor acts in tumor microenvironment to suppress T cell activation
Following the correlations observed, the researchers sought to clarify the possible contributions of HRH1 and its ligand, histamine, to the immune response.
They discovered both proteins were elevated in the tumor microenvironment, but they did not appear to come from the same source. HRH1 was not present in cancer cells but was highly expressed in certain types of TAMs in the tumor microenvironment, known as M2-like macrophages, that contribute to immune suppression. Conversely, cancer cells appear to be a major source of increased histamine levels in patient samples and cancer cell lines.
In preclinical models, blocking HRH1 on macrophages—either by genetic knockout or antihistamine treatment—decreased the immune-suppressive activity of the TAMs, leading to increased T cell activation and inhibition of tumor growth.
To understand how HRH1 in TAMs influences T cell activity, the researchers looked at additional regulatory receptors on the macrophages. Blocking HRH1 activity reduced the membrane localization of VISTA, an inhibitory receptor known to suppress T cell activation. Further, blocking HRH1 caused broad changes in gene expression, resulting in a shift from M2-like features to a more pro-inflammatory state consistent with M1-like macrophages.
The mechanistic data demonstrated that HRH1 acts in TAMs to drive cells toward an immune-suppressive M2-like state and to increase membrane expression of the inhibitory checkpoint VISTA, ultimately leading to dysfunctional T cells and a suppressed anti-tumor response.
Targeting HRH1 enhances checkpoint blockade responses in preclinical models
In preclinical models of breast cancer and melanoma, combining an antihistamine with checkpoint blockade enhanced therapeutic efficacy and prolonged survival over checkpoint blockade alone. Additionally, the antihistamine achieved similar responses in preclinical models as treatment with anti-VISTA antibodies, which are currently being evaluated in clinical trials.
Further, the researchers used a preclinical model of allergic disease to investigate the effects on tumor progression. After allergies were induced, histamine levels and tumor growth increased relative to controls. However, these effects could be reversed with antihistamine treatment.
Similarly, the researchers demonstrated a correlation between plasma histamine levels in patients with cancer and responses to immune checkpoint inhibitors. These findings suggest that elevated histamine levels, either from allergies or cancer cell production, may contribute to suppression of the anti-tumor response.
“Our preclinical findings suggest that antihistamines have the potential to enhance responses to immunotherapy, especially in those with high levels of histamine in the blood,” said corresponding author Dihua Yu, M.D., Ph.D., chair ad interim of Molecular & Cellular Oncology. “There is more work to be done, but we are excited to continue exploring possible therapeutic applications with antihistamines, which offer an inexpensive approach with minimal side effects.”
Source: Read Full Article
