A recent study published in the journal Cellular & Molecular Immunology shows that a new A.30 variant of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) can evade vaccine-induced antibodies and might spread outside the lungs extraordinarily well, with important implications for our public health response.
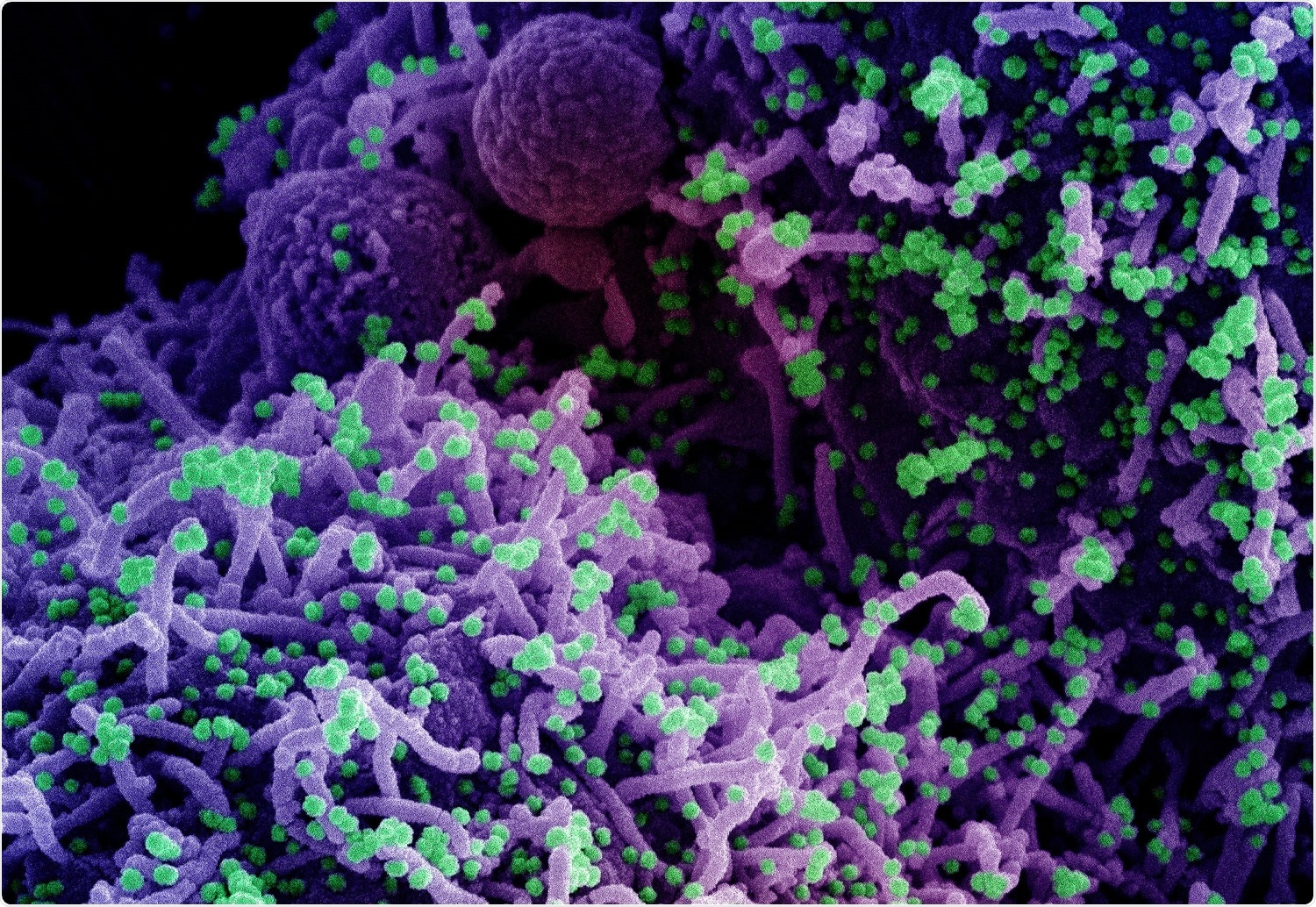
The coronavirus disease (COVID-19) pandemic, caused by the SARS-CoV-2, still rages in many countries around the world, putting significant strains on health systems and economies around the world. One of the main steps towards the end of the pandemic is the use of vaccines.
In a nutshell, COVID-19 vaccines elicit the production of antibodies that are directed against the viral spike glycoprotein, which in turn neutralize the virus. A similar antibody response is seen after natural SARS-CoV-2 infection and these antibodies aid in the protection against severe forms of the disease and death.
Nevertheless, the emergence of SARS-CoV-2 variants that harbor mutations in the spike glycoprotein may resist neutralization by antibodies, compromising vaccine efficacy. Moreover, emerging viral variants with improved transmission properties (most likely due to modified virus-host cell interactions) might swiftly spread globally.
This is why a research group from Germany (led by Dr. Prerna Arora from the Georg-August-University Göttingen) decided to investigate antibody-mediated neutralization and cell entry specific for variant A.30 (also known as A.VOI.V2) detected in spring 2021 in several patients in Angola and Sweden, with likely origins from Tanzania.
In vitro comparisons of SARS-CoV-2 variants
In order to analyze viral cell entry and its inhibition by antibodies, the researchers have employed rhabdoviral pseudotypes with SARS-CoV-2 spike glycoprotein. As targets, they have used kidney-derived 293T and Vero cells, lung-derived A549 and Calu-3 cells, liver-derived Huh-7 cells, and colon-derived Caco-2 cells.
Furthermore, in order to compare A.30 with other SARS-CoV-2 variants, the scientists have analyzed Beta (B.1.351) and Eta (B.1.525) variants. The reason was that these two variants were initially discovered in Africa (akin to A.30), and B.1.351 is considered a salient variant of concern – with the highest level of neutralization resistance among all the variants known to date.
It also has to be emphasized that, in comparison to the spike glycoprotein of the SARS-CoV-2 B.1 variant that was known to circulate during the early phase of the COVID-19 pandemic, the spike glycoprotein of the A.30 variant carries ten amino acid substitutions and five deletions.
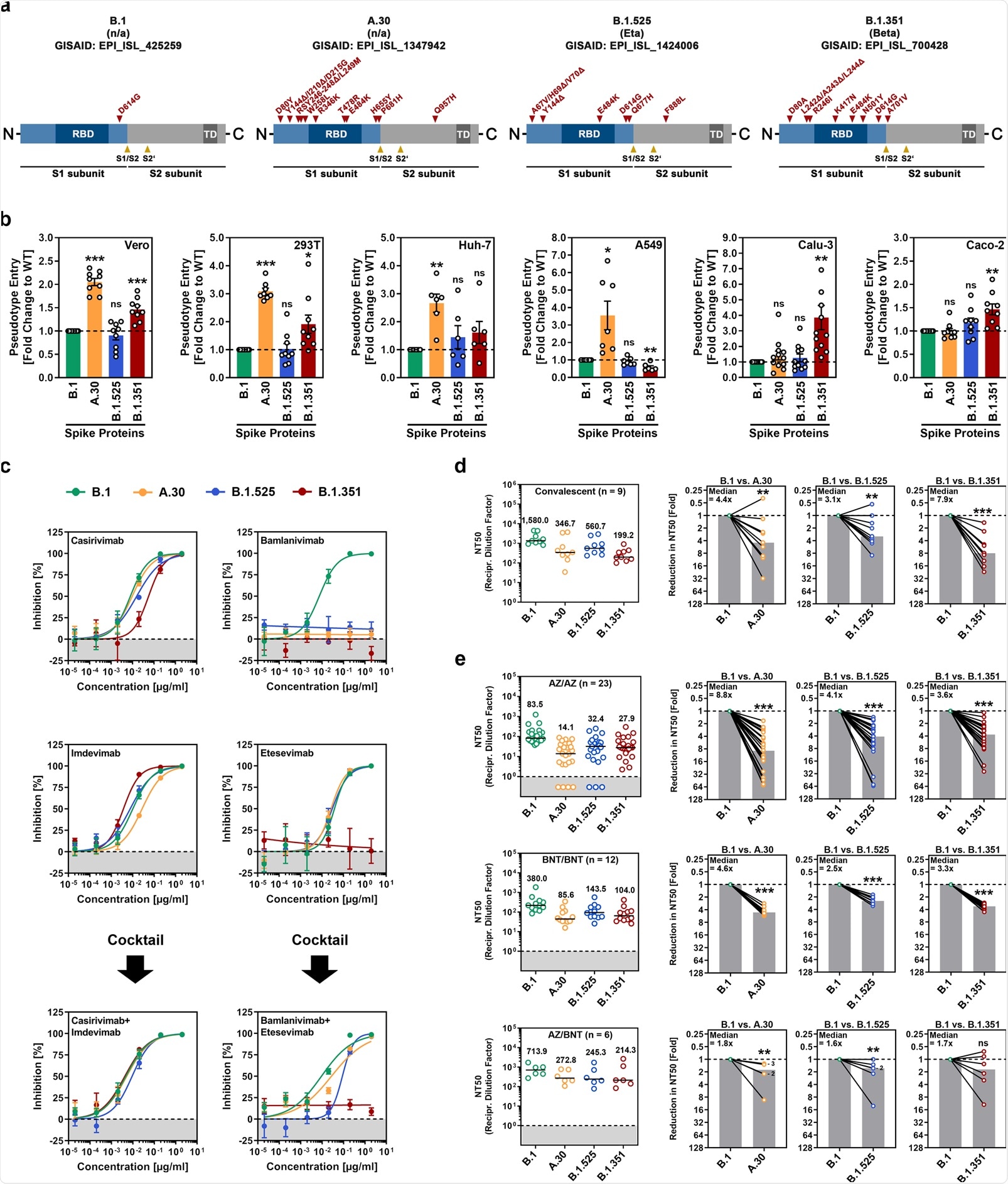
Robust cell entry and neutralization resistance
This study has shown that A.30 has a cell line preference that is not seen with other viral variants. Furthermore, this specific variant can efficiently evade neutralization by antibodies that have been elicited by Astrazeneca-Oxford (AZD1222) or Pfizer-BioNTech (BNT162b2) vaccines.
As SARS-CoV-2 entry into cell lines highly depends on the activation of spike glycoprotein by the cellular proteases cathepsin L or TMPRSS2 (with the latter supporting viral spread in the lungs), it is of particular interest that enhanced A.30 entry was seen for cell lines with cathepsin L (i.e., 293 T, Vero, A549 and Huh-7 cells) – but not for TMPRSS2-dependent entry (i.e., Calu-3 and Caco-2 cells).
In addition, such improved cell line entry was combined with notable resistance to antibodies after AstraZeneca-Oxford or Pfizer-BioNTech vaccination. Neutralization resistance of A.30 exceeded that of the Beta (B.1.351) variant, which was already very resistant to neutralization in cell culture and less well inhibited by the AstraZeneca-Oxford vaccine compared to the Alpha variant.
Public health answer to the variant conundrum
Overall, these results imply that the SARS-CoV-2 variant A.30 can successfully evade control by vaccine-induced antibodies and might have an increased capacity to enter cells in a cathepsin L-dependent manner, which might open the door for viral dissemination outside the lungs.
“As a consequence, the potential spread of the A.30 variant warrants close monitoring and rapid installment of countermeasures”, warn the authors of this study.
However, heterologous vaccination with both above-mentioned vaccines was previously shown to boost neutralizing antibody responses against variants of concern compared to corresponding homologous vaccinations; hence, this might offer robust protection against the A.30 variant as well. In any case, further studies are needed to address this critical public health issue.
- Arora, P. et al. (2021). The spike protein of SARS-CoV-2 variant A.30 is heavily mutated and evades vaccine-induced antibodies with high efficiency. Cellular & Molecular Immunology. https://doi.org/10.1038/s41423-021-00779-5, https://www.nature.com/articles/s41423-021-00779-5
Posted in: Medical Research News | Disease/Infection News
Tags: Amino Acid, Antibodies, Antibody, Cell, Cell Culture, Cell Line, Convalescent Plasma, Coronavirus, Coronavirus Disease COVID-19, Efficacy, Glycoprotein, Health Systems, Homologous, immunity, Immunology, in vitro, Kidney, Liver, Luciferase, Lungs, Pandemic, Protein, Public Health, Receptor, Research, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spike Protein, Syndrome, Vaccine, Virus

Written by
Dr. Tomislav Meštrović
Dr. Tomislav Meštrović is a medical doctor (MD) with a Ph.D. in biomedical and health sciences, specialist in the field of clinical microbiology, and an Assistant Professor at Croatia's youngest university – University North. In addition to his interest in clinical, research and lecturing activities, his immense passion for medical writing and scientific communication goes back to his student days. He enjoys contributing back to the community. In his spare time, Tomislav is a movie buff and an avid traveler.
Source: Read Full Article
