The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) emerged at the end of 2019 to cause the worldwide outbreak of coronavirus disease 2019 (COVID-19). The virus caused over 4.76 million deaths and overwhelming numbers of hospitalizations for serious respiratory distress. While antibodies to the virus are linked to active immunity against the condition, the decline in antibody levels with time is a pressing concern.
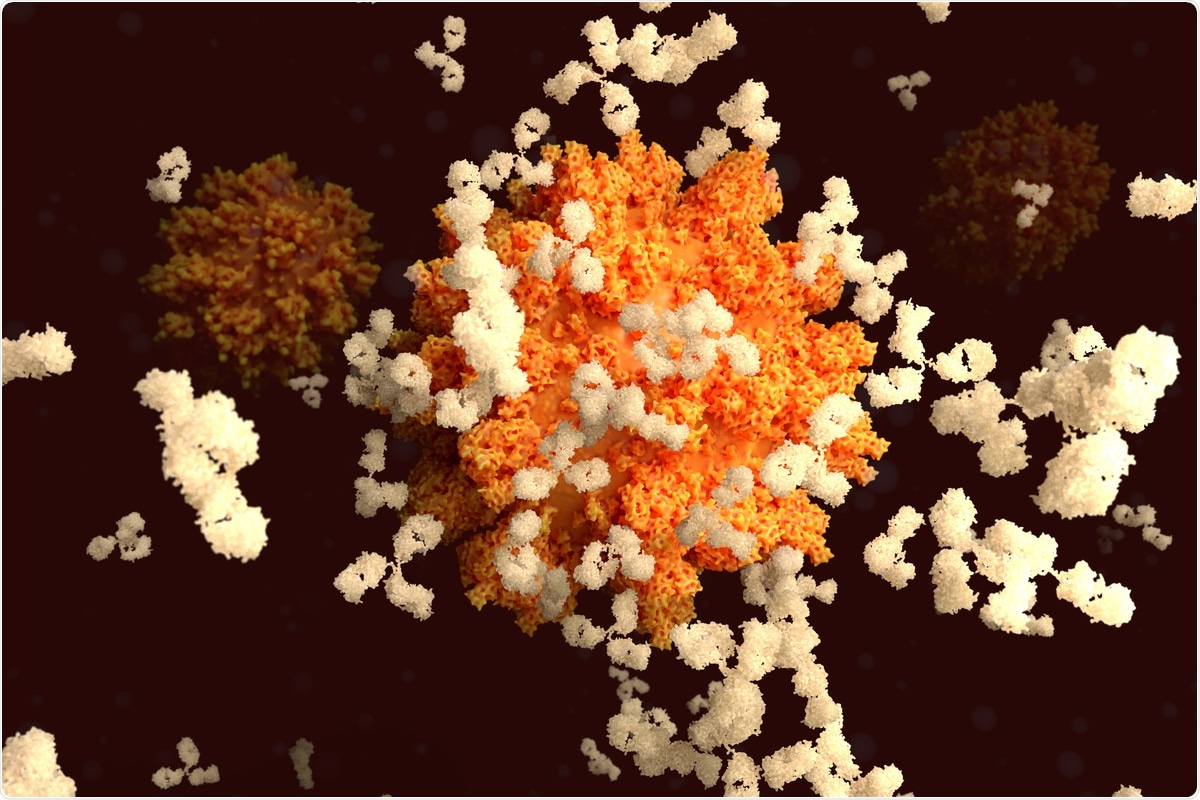 Study: The kinetic of SARS-CoV-2 antibody (Ab) decline determines the threshold for Ab persistence up to one year. Image Credit: Juan Gaertner/ Shutterstock
Study: The kinetic of SARS-CoV-2 antibody (Ab) decline determines the threshold for Ab persistence up to one year. Image Credit: Juan Gaertner/ Shutterstock
A new preprint describes the causal role of waning antibody titers in decreased antibody persistence at one year. A preprint version of the study is available on the medRxiv* server, while the article undergoes peer review.
Background
In response to the extensive and rapid spread of the virus across international and national boundaries, governments clamped down on travel and public interactions, issued lockdown orders, and mandated masks in public worldwide. However, the exact mix differed from region to region. The economic devastation caused by these interventions has been a strong driver of vaccine development to arrest further damage from the pandemic.
Prior infection with the virus has been considered one route to achieve protective immunity; vaccination against the virus is another. However, many studies indicate that antibody titers to the viral spike protein consistently wane over time. This could suggest that booster vaccination is required to maintain protection after a specific period.
The current paper is based on an earlier observation that neutralizing antibodies (nAbs) to the SARS-CoV-2 receptor-binding domain (RBD) are found in the blood for six months or more after natural infection, even when the infection was mild or asymptomatic.
This follow-up study included 12 individuals with a history of mild COVID-19, with a positive neutralization test titers of >1:10. The investigators looked at the number of subjects with persistent antibodies at one year, T cell reactivity to viral antigens, and the presence of memory B cells.
What did the study show?
At one year, the scientists found positive neutralization test titers > 1:10 in 1/12 individuals, approximately 60%. These subjects also had immunoglobulin G (IgG) antibodies to the S1 subunit of the viral spike antigen at > 1:50 BAU/mL and showed inhibition of binding > 36% in a surrogate-virus neutralization test (sVNT).
All subjects were positive for RBD antibodies at this time, but IgG targeting the nucleocapsid (NP) antigen was negative after six months.
The antibody titers at three months and one year were plotted to determine the point at which SARS-CoV-2 antibodies would persist. This showed that when the half-maximal neutralizing titers (NT50) were >1:10 at three months, they persisted at one year. The same was true of anti-S1 IgG >1:60 BAU/mL.
The explanation offered for this association is the pattern of antibody titers in the blood. It is thought to occur in two stages. An initial rapid decline begins after peak antibody levels are attained, a few weeks after vaccination, or after the person recovers from natural infection.
A few months after infection, the second phase of slow decline is observable. Accordingly, the NT50 titers showed a close relationship with anti-S1 IgG and sVNT titers in both phases, as did anti-nucleocapsid IgG ratios. Anti-RBD antibodies diverged slightly, increasing up to 3 months, for the most part, followed by a small drop for a year.
The NT50 titers, anti-S1 IgG titers, and S1-directed B memory cells are closely correlated at the one-year time point, but not S1-targeting gamma-interferon (IFN-y) and interleukin -2 (IL-2) levels. The latter was higher in those with lower antibody levels and memory B cell counts.
What are the implications?
It is important to know how long antibody responses may be expected to persist in a given individual after natural infection with SARS-CoV-2. According to the findings of this study, antibody titers at three and six months are key metrics in determining antibody persistence. However, the latter also depends on the initial peak antibody titer.
Earlier studies have suggested that RBD-specific memory B cells and antibodies persist at stable levels at 6-12 months from infection. The current paper adds a link between persistent antibody levels and the trajectory of NT50 and S1-specific IgG titers.
The researchers suggest "S1-specific IgG concentrations of 60 BAU/ml three months post-infection as a potential threshold to predict maintenance of neutralizing Ab levels for one year." This measure is more easily determined on a routine basis than the NT50.
The memory B cell's response to the spike antigen has been earlier reported to be associated with a higher vaccine response, probably due to a booster response from the memory B cells. Neutralizing antibody responses were not consistently associated with spike-specific T cell recall responses, however.
Overall, the study concludes,
Our data suggest that a threshold of Ab levels can be identified three months after (even) mild infection predicating persistence of SARS-CoV-2 specific Ab levels up to one year."
Since neutralizing antibodies and binding antibodies to the spike antigen are linked to vaccine-induced protection, and since antibodies show a similar rate of decline after infection or vaccination, this threshold may help identify those likely to be protected by the vaccine as well, all the more since vaccination studies have not yielded any useful measure of protective immunity.
*Important notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information
Garner-Spitzer, E. et al. The Kinetic Of SARS-Cov-2 Antibody (Ab) Decline Determines the Threshold for Ab Persistence Up to One Year. medRxiv preprint. doi: https://doi.org/10.1101/2021.09.20.21263172. https://www.medrxiv.org/content/10.1101/2021.09.20.21263172v1
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: Antibodies, Antibody, Antigen, B Cell, Blood, Cell, Coronavirus, Coronavirus Disease COVID-19, immunity, Immunoglobulin, Interferon, Interleukin, Pandemic, Protein, Receptor, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spike Protein, Syndrome, Vaccine, Virus

Written by
Dr. Liji Thomas
Dr. Liji Thomas is an OB-GYN, who graduated from the Government Medical College, University of Calicut, Kerala, in 2001. Liji practiced as a full-time consultant in obstetrics/gynecology in a private hospital for a few years following her graduation. She has counseled hundreds of patients facing issues from pregnancy-related problems and infertility, and has been in charge of over 2,000 deliveries, striving always to achieve a normal delivery rather than operative.
Source: Read Full Article
