Cancer-associated genes called oncogenes are well known to stimulate cell growth and division—causing tumors to balloon and spread. But now, researchers at the Stanford School of Medicine and Sarafan ChEM-H have found that one notorious oncogene called Myc also has a direct role in disguising growing cancers from the immune system.
Myc is associated with more than 70% of human cancers, and blowing these cancers’ cover could lead to a new class of cancer therapy, the researchers believe.
They found that a key component of the Myc-induced camouflage is a sugar molecule coating on the surface of cancer cells. This sugar sends a “stand down” signal to immune cells called macrophages that would normally engulf and destroy the cancer cells.
The discovery links two seemingly unrelated previous observations: Cancer cells differ from healthy cells in the patterns of sugars on their surface, and the Myc oncogene somehow protects cancer cells from the immune system by increasing the production of specific proteins in the cells. Deciphering the connection required the collaboration of two labs, one run by sugar chemist and recent Nobel Prize winner Carolyn Bertozzi, Ph.D., and another headed by cancer expert Dean Felsher, MD, Ph.D.
“I think this is very likely to lead to an entirely new line of cancer therapeutics,” said Felsher, a professor of medicine and of pathology. Felsher also directs the Stanford Translational Research and Applied Medicine Center, which encourages physicians and basic scientists to collaborate to bring their results into the clinic. “Many cancer treatments were developed, essentially, through trial and error, but this is completely different. We know the mechanism and exactly how to target this process.”
“It’s a striking connection,” said Bertozzi, the Anne T. and Robert M. Bass Professor in the School of Humanities and Sciences. “My lab had been trying to understand why cancer cells have altered patterns of sugars on their surfaces, and how these changes help the cells escape the immune system. Now we know that Myc regulates the production of proteins that make these sugar molecules that trick the immune system into ignoring the cancer cells.”
Felsher and Bertozzi, who is the Baker Family Director of Sarafan ChEM-H, are the senior authors of the research, which was published online March 10 in the Proceedings of the National Academies of Sciences. Graduate student Benjamin Smith and instructor Anja Deutzmann, Ph.D., are the lead authors of the study.
Genes gone astray
Oncogenes are good genes gone bad. Before they go to the dark side, they play a critical role in controlling how and when a cell divides. But when they are mutated or freed from the normally tight layers of regulation a cell uses to moderate their activity, they spur rapid cell division and tumor growth.
Like many oncogenes, Myc is a member of a class of proteins called transcription factors. Transcription factors are master regulators that adjust the level of many proteins in the cell up or down in response to external and internal signals. These proteins can spur a cell to ignore signals to stop dividing, or sidestep built-in cellular suicide programs meant to do away with misbehaving cells. They can also modulate the cell’s external environment, coaxing unfriendly neighbors into alliances, or facilitating the growth of new blood vessels to deliver much-needed oxygen to a growing tumor. In short, they are perfectly poised to wreak havoc when they go awry.
Felsher has spent decades studying how Myc triggers cancerous changes inside and outside a cell. Early in his career, he started to suspect that Myc also tamped down the immune system—a relatively new idea at the time.
Bertozzi is an expert in analyzing the patterns of sugars, or glycans, that bristle from the surfaces of every living cell. These sugars are dizzyingly complex in their structures, and they mediate critical interactions with other cells, signaling molecules like hormones and pathogens like viruses and bacteria. They require specialized knowledge and equipment to study thoroughly, and Bertozzi is a world leader in the field.
Felsher and Deutzmann, then a postdoctoral scholar in Felsher’s lab, had learned that Myc likely controlled the expression of a type of protein called a glycosyltransferase, which is necessary to build complex molecules including sugars on the surface of cells. But they didn’t have the tools or expertise to pursue the finding.
But in the summer of 2016, Felsher invited Bertozzi to speak at a symposium for his Translational Research and Applied Medicine center. Bertozzi, who had recently arrived at Stanford University, accepted the offer enthusiastically.
“I came to Stanford with the high hopes that I could interact directly with physicians and learn more about human disease,” Bertozzi said. “They know more about biology than I ever have. So I was very excited when Dean asked me to speak. I thought, ‘There will be a bunch of doctors there!’ This was a totally new thing for me.”
At the symposium, Bertozzi spoke about an observation in her lab that she’d been pondering.
“We know, and have known for some time, that there are changes in the patterns of sugar molecules on the surface of cancer cells, and we wondered if there were opportunities for new therapies based on these changes,” she said.
As she spoke, the atmosphere in the room changed. “Our students got together after the talk and said, ‘This all makes sense,'” Felsher recalled. “I got goosebumps,” Bertozzi said, after hearing from Felsher and his lab members about the link between Myc and glycosyltransferase enzymes. “We realized this must be how the sugars are changing.”
The labs immediately agreed to collaborate, with Deutzmann and the Felsher lab providing the information about Myc and its role as an oncogene, and Smith and the Bertozzi lab contributing the expertise in sugar science, also called “glycobiology.”
Ferreting out Myc’s role
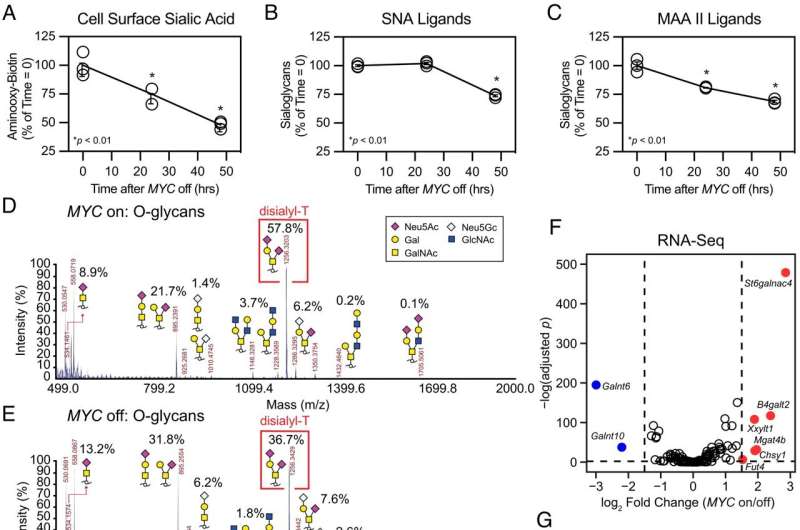
Together, the labs discovered that Myc drives the production of a glycosyltransferase called ST6GalNAc4, which is necessary to make a sugar molecule called disialyl-T that pops up in abundance on the surface of Myc-driven cancer cells. Disialyl-T binds to another molecule on the surface of macrophages, flipping them in one fell swoop from foe to friend.
This interaction is important; leukemia cells driven by Myc expression, but unable to make ST6GalNAc4, grew more slowly in laboratory mice and generated a stronger immune response to the tumor than cells that could make ST6GalNAc4. Additionally, Smith and Deutzmann found that people with cancers that have high levels of both Myc and ST6GalNAc4 have a poorer prognosis and fewer immune cells near their tumors than those with lower levels.
“This connection between Myc and sugar biology is really spectacular, and it was right in front of everyone’s faces,” Bertozzi said. “We know from Dean’s previous work that Myc regulates cell growth and division, which is obviously important for cancer. But what wasn’t known is that Myc can drive the expression of sugars on the cancer cell surface to allow it to evade recognition by the immune system.”
The researchers are eager to continue their partnership to develop novel new cancer therapeutics.
“The way we see it, there are two next obvious directions of research,” Bertozzi said. “First, we want to test whether other oncogenes are also affecting the sugar structures on the surface of cancer cells. Second, we want to see if we can inhibit ST6GalNAc4 to enhance the ability of macrophages to destroy the cancer cells.”
“What Stanford is doing—intentionally bringing together physicians and basic scientists from diverse fields—is exactly the way we are going to cure disease,” Felsher said.
More information:
Benjamin A. H. Smith et al, MYC-driven synthesis of Siglec ligands is a glycoimmune checkpoint, Proceedings of the National Academy of Sciences (2023). DOI: 10.1073/pnas.2215376120
Journal information:
Proceedings of the National Academy of Sciences
Source: Read Full Article
