A new study suggests that it is possible to design drugs that can target a type of shape-shifting protein involved in Alzheimer’s disease, which was previously thought to be undruggable.
A team of researchers, led by the University of Cambridge, have identified a new mechanism of targeting amyloid-beta, a protein fragment that clumps together and kills healthy brain cells in people with Alzheimer’s disease.
Working with colleagues from Imperial College London, Institut Pasteur, and the University of Florence, the researchers found that it is possible for a drug-like molecule to target amyloid-beta in its disordered state, reducing its ability to form the toxic clusters which are the hallmark of Alzheimer’s disease. The results, reported in the journal Science Advances, could form the basis of a new avenue for the development of potential treatments for the disease.
“Amyloid-beta is a disordered protein, a type of target that is elusive for standard therapeutic approaches,” said Professor Michele Vendruscolo from Cambridge’s Centre for Misfolding Diseases, who led the research. “It is constantly changing shape, so traditional drug discovery techniques don’t work on it. By revealing a new drug-binding mechanism, we have extended traditional drug discovery approaches based on the optimisation of the binding affinity to include disordered proteins.”
Most drugs work by binding proteins through what is often described as a lock-and-key mechanism, where a drug fits into a protein’s grooves like a key in a lock. However, since they are often changing shape, disordered proteins such as amyloid-beta don’t have stable ‘locks’ for drugs to bind to, which is why they are considered ‘undruggable.’
The approach developed by the researchers is based on the so-called disordered binding mechanism that they discovered, where small molecules form a disordered complex with the protein target, so that it is like the protein and the drug are ‘dancing’ with one another.
The researchers characterized this new mechanism using a combination of biophysical experiments, mathematical modeling, in vivo experiments and computation.
First, they tested the aggregation of amyloid-beta in the presence of the compound in in vitro assays. Data from these experiments allowed the researchers to build a mathematical model of how the drug was able to inhibit the aggregation of amyloid-beta at the microscopic level.
The team also used high-performance computing methods to study the binding interaction at the atomic level. These intensive calculations allowed the researchers to ‘see’ how the binding was occurring at the atomic level, which is otherwise almost impossible to observe experimentally. Further tests were then carried out in nematode worms, which are often used as a model organism to study Alzheimer’s disease.
“In contrast to the traditional lock-and-key binding mechanism, in which a drug tightly interacts with its target in a specific conformation, we found that both the small molecule and the disordered protein remained extremely dynamic, and that the small molecule interacted with many parts of the protein,” said Gabriella Heller, Schmidt Science Fellow and the study’s first author.
“This way of stabilizing native states of proteins is a powerful drug discovery strategy, which has so far been extremely challenging for disordered proteins,” said Vendruscolo.
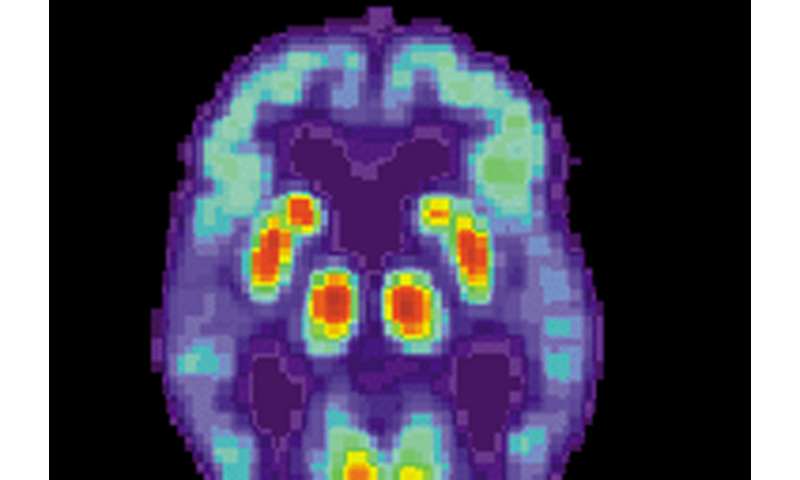
Amyloid beta, the protein which the team targeted, is closely associated with Alzheimer’s disease as it is the primary component of senile plaques, which are characteristically found in the brains of the people affected by the disease.
While this research is still preliminary in terms of clinical translation, it demonstrates that targeting the formation of these plaques by preventing the aggregation of amyloid-beta is a major therapeutic strategy. To date the mainstream approach has been to develop antibodies to bind to the aggregates, promoting their removal and interfering with their self-assembly.
Source: Read Full Article
