A novel artificial intelligence blood testing technology developed by researchers at the Johns Hopkins Kimmel Cancer Center was found to detect over 90% of lung cancers in samples from nearly 800 individuals with and without cancer.
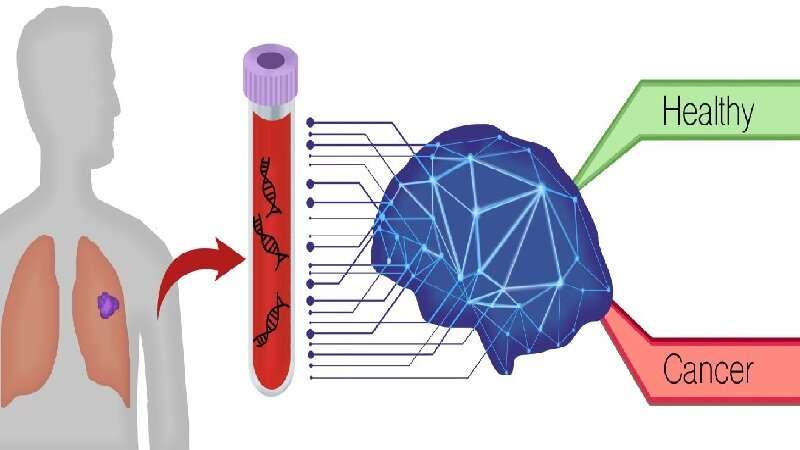
The test approach, called DELFI (DNA evaluation of fragments for early interception), spots unique patterns in the fragmentation of DNA shed from cancer cells circulating in the bloodstream. Applying this technology to blood samples taken from 796 individuals in Denmark, the Netherlands and the U.S., investigators found that the DELFI approach accurately distinguished between patients with and without lung cancer.
Combining the test with analysis of clinical risk factors, a protein biomarker, and followed by computed tomography imaging, DELFI helped detect 94% of patients with cancer across stages and subtypes. This included 91% of patients with earlier or less invasive stage I/II cancers and 96% of patients with more advanced stage III/IV cancers. These results will be published in the August 20 issue of the journal Nature Communications.
Lung cancer is the most common cause of cancer death, claiming almost 2 million lives worldwide each year. However, fewer than 6% of Americans at risk for lung cancers undergo recommended low-dose computed tomography screening, despite projections that tens of thousands of deaths could be avoided, and even fewer are screened worldwide, explains senior study author Victor E. Velculescu, M.D., Ph.D., professor of oncology and do-director of the Cancer Genetics and Epigenetics Program at the Johns Hopkins Kimmel Cancer Center. This is due to a variety of reasons, including concerns of potential harm from investigation of false positive imaging results, radiation exposure or worries about complications from invasive procedures. “It is clear that there is an urgent, unmet clinical need for development of alternative, noninvasive approaches to improve cancer screening for high-risk individuals and, ultimately, the general population,” says lead author Dimitrios Mathios, a postdoctoral fellow at the Johns Hopkins Kimmel Cancer Center. “We believe that a blood test, or ‘liquid biopsy,’ for lung cancer could be a good way to enhance screening efforts, because it would be easy to do, broadly accessible and cost-effective.”
The DELFI technology uses a blood test to indirectly measure the way DNA is packaged inside the nucleus of a cell by studying the size and amount of cell-free DNA present in the circulation from different regions across the genome. Healthy cells package DNA like a well-organized suitcase, in which different regions of the genome are placed carefully in various compartments. The nuclei of cancer cells, by contrast, are like more disorganized suitcases, with items from across the genome thrown in haphazardly. When cancer cells die, they release DNA in a chaotic manner into the bloodstream. DELFI helps identify the presence of cancer using machine learning, a type of artificial intelligence, to examine millions of cell-free DNA fragments for abnormal patterns, including the size and amount of DNA in different genomic regions. This approach provides a view of cell-free DNA referred to as the “fragmentome.” The DELFI approach only requires low-coverage sequencing of the genome, enabling this technology to be cost-effective in a screening setting, the researchers say.
For the study, investigators from Johns Hopkins, working with researchers in Denmark and the Netherlands, first performed genome sequencing of cell-free DNA in blood samples from 365 individuals participating in a seven-year Danish study called LUCAS. The majority of participants were at high risk for lung cancer and had smoking-related symptoms such as cough or difficulty breathing. The DELFI approach found that patients who were later determined to have cancer had widespread variation in their fragmentome profiles, while patients found not to have cancer had consistent fragmentome profiles. Subsequently, researchers validated the DELFI technology using a different population of 385 individuals without cancer and 46 individuals with cancer. Overall, the approach detected over 90% of patients with lung cancer, including those with early and advanced stages, and with different subtypes. “DNA fragmentation patterns provide a remarkable fingerprint for early detection of cancer that we believe could be the basis of a widely available liquid biopsy test for patients with lung cancer,” says author Rob Scharpf, Ph.D., associate professor of oncology at the Johns Hopkins Kimmel Cancer Center.
Source: Read Full Article
