Researchers at the Francis Crick Institute have identified visual changes in the bone marrow caused by acute myeloid leukemia (AML). The imaging technique used is now being tested in hospital to see if it could help predict whether different treatments will be effective in individual patients.
Acute myeloid leukemia (AML) is a type of blood cancer that starts from young white blood cells called granulocytes or monocytes in the bone marrow. It is the most common acute leukemia in adults, with around 3,100 people diagnosed each year in the UK.
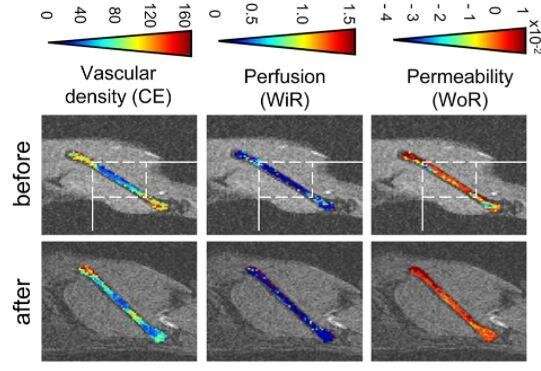
In their study, published in Haematologica, the scientists used an imaging technique, Dynamic contrast-enhanced (DCE)-MRI, in mice to see how this cancer affects the bone marrow blood vessels. The technique is particularly useful for measuring blood flow and permeability of different tissues but is not currently routinely used in hospitals to monitor leukemia.
They found that there was decreased blood flow in the bone marrow of mice with AML in comparison to healthy mice.
The team are now working with Barts Health Trust to test whether this imaging method could be a useful tool for doctors. By imaging patients before and after treatment, they hope to identify patterns in the images which could be used to predict if a patient will respond to a particular treatment. For example, those with severely reduced blood flow in the bone marrow, might not respond as well to chemotherapy, as the drugs are less likely to reach their cancer cell targets.
It could also help doctors identify patients at high risk of relapse. This is because reduced blood flow is a sign that the cancer cells have surrounded themselves with a protective microenvironment which helps the cancer cells evade or ‘hide’ from the treatment.
Dominique Bonnet, author and group leader of the Haematopoietic Stem Cell Laboratory at the Crick, says: “The DCE-MRI imaging technique has existed for over 20 years but is not often used in the clinic due to a lack of image standardization and analysis tools. By developing these tools for AML, we hope to have opened the door for this non-invasive imaging to be used by doctors treating patients with this type of cancer and maybe other conditions too.”
The team also used the imaging technique to monitor whether chemotherapy was able to improve blood flow in the bone marrow. They saw that the treatment had different effects in mice which were infected with AML cells from different patients, reflecting the diverse nature of the disease. In some cases, the treatment partially improved blood flow, while in others it made it worse.
Ana Gomes, lead author and senior scientist in the Haematopoietic Stem Cell Laboratory at the Crick, says: “A difficulty in treating AML is that it does not behave the same in everyone. It might affect different parts of the tissue and while some patients may respond well to a given treatment, others do not. Helping doctors to better match patients with the treatment most likely to work for them would be a real benefit for patients and their families.”
The work also identified how the bone marrow is affected by aging, with older mice showing a deterioration in vascular permeability. This is the capacity of a blood vessel to allow for molecules to flow in and out of it.
Source: Read Full Article
