Scientists at Vanderbilt University Medical Center (VUMC) and the Translational Genomics Research Institute (TGen) in Phoenix, Arizona, have discovered previously unreported genetic and cellular changes that occur in the lungs of people with pulmonary fibrosis (PF).
Their findings, reported Wednesday, July 8, in the journal Science Advances, should aid the search for new ways to treat or prevent this devastating lung-scarring disease, they said.
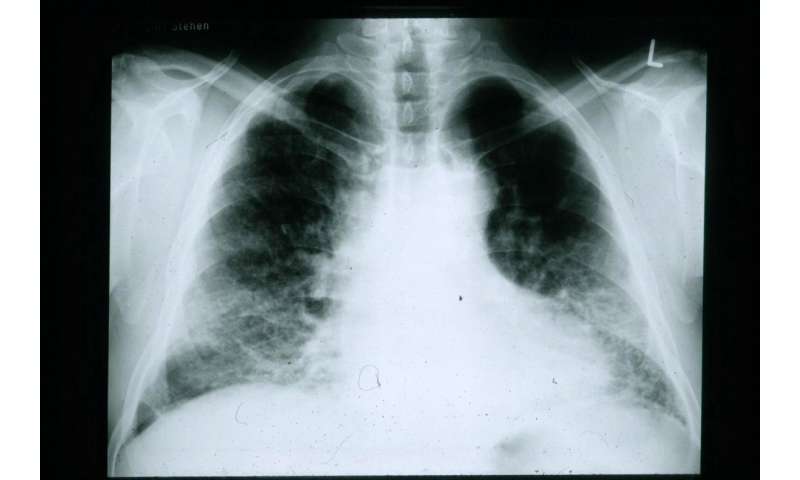
PF can be triggered by inhaling coal or asbestos, exposure to radiation and certain drugs and hypersensitivity and autoimmune reactions. In addition, “idiopathic” PF, a subset of the disease with no known cause, kills up to 40,000 Americans each year, according to the Pulmonary Fibrosis Foundation.
Anti-fibrotic and anti-inflammatory drugs can slow disease progression, but they are not without serious side effects. Lung transplantation is another option, but due to the severe shortage of donor organs few people with PF or IPF obtain new, healthy lungs.
“Our understanding of the cellular and molecular mechanisms actively driving disease in the lungs of pulmonary fibrosis patients has been limited,” said Jonathan Kropski, MD, who led the study with TGen’s Nicholas Banovich, Ph.D. “We have not yet been able to answer very basic questions, such as ‘Which cells are the ones that make the fibrosis?'”
Kropski is assistant professor of Medicine and Cell and Developmental Biology in the Division of Allergy, Pulmonary and Critical Care Medicine at VUMC.
The researchers used advanced microfluidic techniques and single-cell RNA sequencing to identify variations in the transcriptome, or gene-expression profile, in more than 100,000 individual lung cells from 20 patients with PF and 10 controls who did not have the disease.
They identified multiple previously undescribed types of cells from patients with PF that expressed high levels of collagen and other components of the extracellular matrix (ECM) that accumulates in PF lungs.
Normally the ECM provides the structural and biochemical support between cells that are organized into tissues. But in PF and IPF, the progressive accumulation of ECM destroys the alveoli, the tiny air sacs in the lungs that allow for the exchange of oxygen and carbon dioxide.
Using another technique, RNA in situ hybridization, the researchers mapped the distribution of various cell populations in PF lungs compared to control lungs. Taken together, these findings “provide remarkable insights into the cellular architecture of the human lung and the fundamental mechanisms driving disease pathology in PF,” they conclude.
Source: Read Full Article
