In a clinical trial testing whether a daily regimen of hydroxychloroquine could protect those most likely to be exposed to COVID-19, researchers from the Perelman School of Medicine at the University of Pennsylvania found there was no difference in infection rates among health care workers who took the drug versus those taking a placebo. While the researchers observed a lack of effect associated with hydroxychloroquine, infection levels were low among the participants, which the researchers believe points to the effectiveness of other prevention measures in the health system: social distancing, use of personal protective equipment, and proper hand hygiene. The study was published today in JAMA Internal Medicine.
“This work represents the first randomized trial of hydroxychloroquine’s prophylactic effect for those not yet exposed to COVID-19,” said the study’s lead author, Benjamin Abella, MD, MPhil, a professor of Emergency Medicine and the director of Penn Medicine’s Center for Resuscitation Science. “And while hydroxychloroquine is an effective drug for the treatment of diseases like lupus and malaria, we saw no differences that would lead us to recommend prescribing it as a preventive medication for COVID-19 in front line workers.”
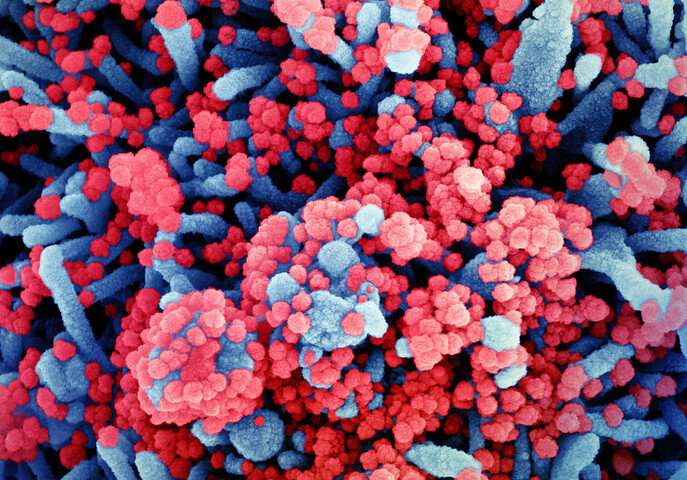
Due to the novel nature of COVID-19, the science and medical communities have had to rapidly assess treatment and prevention measures. One drug that has been considered as a potential preventive solution was hydroxychloroquine, based on laboratory studies that it could prevent SARS-CoV-2, the virus that causes COVID-19, from entering cells in tissue culture.
As such, Abella, along with the study’s senior author Ravi Amaravadi, MD, an associate professor of Medicine in Hematology-Oncology and the program co-Leader of Cancer Therapeutics at the Abramson Cancer Center, and their co-authors set out to rigorously test whether taking a substantial dose of hydroxychloroquine—600 milligrams daily for two months- would have an effect on infection rates. They conducted this study among hospital workers that regularly came into contact with COVID-19 patients.
The researchers were able to analyze a pool of 125 physicians, nurses, certified nursing assistants, emergency technicians, and respiratory therapists that they recruited for the study. This population worked in several different areas of the two University hospitals, including the emergency departments and COVID-19 units. Roughly half of the participants in the study took hydroxychloroquine while the other half took a matching placebo (a cellulose pill). The study was double-blinded, meaning neither the researchers, nor the participants knew which drug they were assigned.
Extensive testing was used to rigorously prove who did or did not contract the virus. Each person received swab and antibody testing for COVID-19 at the start of their participation in the study, halfway through, and at the end—an eight-week span during the study period that began April 9 and ended July 14, 2020. Participants also had electrocardiogram (ECG) tests because of concerns about hydroxychloroquine causing heart rhythm problems in severe cases of COVID-19.
“To really test the potential of HCQ as a prevention drug, we felt it was key to recruit health care workers with many hours of direct physical exposure to COVID-19 patients, then randomize them in a double-blind manner between hydroxychloroquine or a matching placebo, and treat them for a long period of time,” said Amaravadi. “Through that whole time, we monitored participants closely for their safety.”
At the end of the study, 6.3 percent of those who took the hydroxychloroquine had tested positive for COVID-19 while 6.6 percent of those who took the placebos were positive. None required hospitalization. Additionally, there was no difference detected in the heart rhythms between those in either arm of the study, which showed that while the drug had no preventive effect, it was also not detrimental, outside of some temporary side effects like diarrhea for some.
“The differences we saw were negligible,” Amaravadi said. “And those who did get the virus, whether they were taking hydroxychloroquine or not, were all asymptomatic or had very mild forms of COVID-19.”
While the study was originally slated to recruit 200 health care workers, an analysis along the way showed that a continuation of enrollment would not yield different results. An independent data safety and monitoring board reviewed the findings and concurred.
Source: Read Full Article
