Before COVID, there was Zika. In 2015, the number of babies born in Brazil with small heads and brains—a condition known as microcephaly—suddenly increased dramatically. The severe deformities left the children disabled for life, and caused intense global concern.
These cases of microcephaly were soon shown to be caused by pregnant women being infected with the mosquito-borne Zika virus. The virus infects and kills cells that form the brain, hampering its proper development.
But the impact was not universal—certain regions in north-eastern Brazil saw far more cases of microcephaly than others.
Scientists began to question whether other factors might be at play that intensified the epidemic in some places. Not long after, they focused their attention on pyriproxyfen, a globally approved pesticide used against household insects in agriculture—including mosquitoes. Pyriproxyfen was used intensively in the regions with the highest numbers of microcephaly cases.
Now, in a new study, we have shown that pyriproxyfen could indeed exacerbate the already severe effects the Zika virus has on fetal brain development.
Pyriproxyfen and Zika
In late 2014, pyriproxyfen was introduced to drinking water throughout Brazil to control the Aedes aegypti mosquito population, which spreads the Dengue and Zika viruses.
But the insecticide is known to accumulate in the environment for years, eventually finding its way into the human body. So to prevent potential side-effects, the World Health Organisation had recommended the daily intake of pyriproxyfen should not exceed 0.3 mg/L for an average adult, and concentrations in drinking water should be lower than 0.01 mg/L.
As babies and fetuses generally absorb or accumulate more chemicals than adults, they can be at greater risk. And because there was a strong geographical overlap between the use of pesticides and microcephaly cases, even these small doses raised issues concerning safety.
Epidemiological and experimental studies have since delivered contradictory results regarding whether or not pyriproxyfen was implicated in the disease outbreak. But in our recently published study, we discovered that pyriproxyfen impairs thyroid hormone signaling in the brain, modifying crucial processes for its proper development.
How pyriproxyfen affects brain development
Thyroid hormone is an important molecule that helps shape the fetal brain. Without it, the brain doesn’t grow as it’s supposed to, leaving affected children with learning difficulties for life.
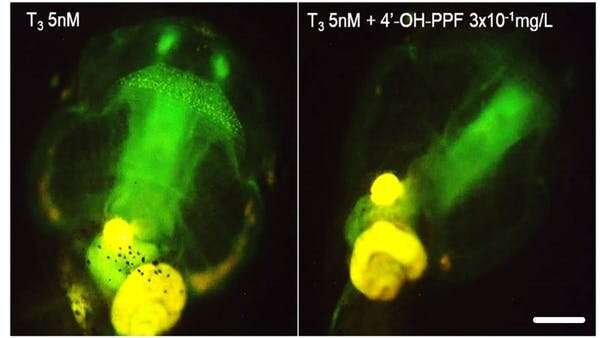
In the lab, we house genetically modified tadpoles that emit green fluorescence when exposed to thyroid hormone. More thyroid hormone means more green signal, indicating the hormone is active in the tadpoles’ cells.
When we exposed our tadpoles to pyriproxyfen, the green signal dropped dramatically. This demonstrated that the pesticide blocks thyroid hormone action.
One of the most important roles of thyroid hormone is to generate a balanced amount of nerve cells and their supporting cells, known as glia. Together, they form the essential building blocks of the brain.
Since pyriproxyfen blocks normal thyroid hormone action, we thought it might affect the generation of neurons and glial cells too. To investigate this, we used stem cells cultured from mouse brains, and exposed them to increasing doses of the pesticide.
The findings were clear: the higher the dose, the fewer cells were generated, and the more they died, producing an unbalanced proportion of nerve cells and glia.
The brains of the exposed tadpoles in our study did not develop normally, and made them behave unnaturally. Underlying these changes were altered expression patterns of a number of genes.
A key player in this was the gene Msi1, which encodes a protein called Musaschi-1. The Zika virus uses this protein to replicate and infect other cells, and we knew from previous studies that more thyroid hormone resulted in less Musaschi-1.
Not surprisingly, the cells that survived pesticide exposure contained much more of the protein due to blocked thyroid hormone action. That’s why we hypothesized that, through increasing Musaschi-1, pyriproxyfen could allow the virus to replicate faster.
To test this, we infected exposed stem cells with the Zika virus and found that the transcription of key genes was altered compared to when they were infected with the virus alone and not exposed to the pesticide. Although we didn’t observe higher infection rates, it’s still possible that pesticide exposure could aggravate hampered brain development. That can worsen the impact the virus has on a child’s later-life intellectual capacities, and requires further investigation.
Regulating pesticides
This is not the first time a pesticide has been shown to alter the course of a disease.
For example, individuals with higher amounts of another chemical that disrupts the endocrine system, perfluorobutanoic acid, in their blood, are at risk of a more severe course of COVID-19.
But for many other ubiquitous pesticides to which we are continuously exposed in our daily life, we have no clue as to how they affect us, and whether they interact with viral diseases.
We need better testing protocols for pesticides to obtain more solid data to inform health policies and decision makers.
As for pyriproxyfen, Europe is not proposing to use it at concentrations advised by the World Health Organization, but recently reauthorised it.
Source: Read Full Article
