Pulmonary arterial hypertension (PAH) is a type of high blood pressure in the lungs, in which blood vessels are narrowed, blocked or destroyed, causing the heart to work harder and, in time, result in cardiac weakness and failure.
The disease is relatively rare, but affects an estimated 100,000 persons in the United States, and results in 20,000 deaths annually. There is no cure.
In a study published May 4, 2022 in Science Translational Medicine, researchers at the University of California San Diego School of Medicine describe the underlying signaling pathway that results in PAH—and a novel monoclonal antibody therapy that blocks the abnormal blood vessel formation characterizing the disease.
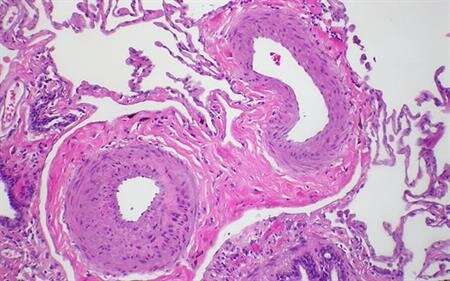
At the cellular level, PAH progresses with proliferation of vascular smooth muscle cells (vSMC) that cause small arteries in the lungs to become narrowed, leading to progressively less oxygen in the blood. A research team, led by senior author Patricia A. Thistlethwaite, MD, Ph.D., professor of surgery in at UC San Diego School of Medicine and a cardiothoracic surgeon at UC San Diego Health, focused on overexpression of the NOTCH ligand JAGGED-1, a binding protein involved in cell signaling and, in this case, the development of small pulmonary vSMCs.
They found that overexpression of the NOTCH3 ligand, JAGGED-1, spurs vSMC proliferation, but the NOTCH3 ligand DELTA-LIKE 4 inhibits it. The researchers then developed a therapeutic monoclonal antibody that selectively blocks JAGGED-1-induced NOTCH3 signaling, effectively reversing pulmonary hypertension in two rodent models of the disease, without toxic side effects.
“These findings reveal two opposing roles of NOTCH ligands,” said Thistlethwaite. “Importantly, it opens the door to a potentially new, safe treatment for PAH, using a monoclonal antibody that selectively inhibits NOTCH3 activation in the lung vasculature.”
Source: Read Full Article
