Disparities in healthcare exist in every specialty. In rheumatology, health disparities look like lack of access to care and lack of education on the part of rheumatologists and their patients, according to a speaker at the 2022 Rheumatology Winter Clinical Symposium.
Health disparities can affect people based on their racial or ethnic group, gender, sexual orientation, a mental or physical disability, socioeconomic status, or religion, Alvin Wells, MD, PhD, director of the department of rheumatology at Advocate Aurora Health in Franklin, Wisconsin, said in his presentation. But a person’s environment also plays a role — “where you live, work, play, and worship.”
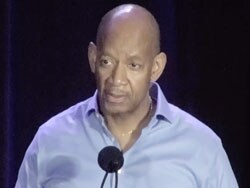
Dr Alvin Wells
Social determinants of health can affect short-term and long-term health outcomes, functioning, and quality of life, he noted. “It’s economic stability, it’s access not only to healthcare, but also to education. And indeed, in my lifetime, as you know, some individuals weren’t allowed to read and write. They weren’t allowed to go to schools. You didn’t get the same type of education, and so that made a dramatic impact in moving forward with future, subsequent generations.”
In a survey of executives, clinical leaders, and clinicians published in NEJM Catalyst Innovations in Care Delivery, 48% said widespread disparities in care delivery were present in their organizations. According to the social psychologist James S. House, PhD, some of these disparities like race/ethnicity, socioeconomic status, genetics, and geography are fixed, while others like psychosocial, medical care/insurance, and environmental hazards are modifiable. While factors like education, work, and location might be modifiable for some patients, others don’t have the ability to make these changes, Wells explained. “It’s not that easy when you think about it.”
Within rheumatology, racial and ethnic disparities exist in rheumatoid arthritis when it comes to disease activity and use of disease-modifying antirheumatic drugs. Disparities in outcomes based on race and geographic location have also been identified for patients with systemic lupus erythematosus, lupus nephritis, and based on race in osteoarthritis and psoriatic arthritis. “Where people live, where they reside, where their ZIP code is,” makes a difference for patients with rheumatic diseases, Wells said.
“We’ve heard at this meeting [about] some amazing drugs in treating our patients, both [for] skin and joint disease, but not everybody has the same kind of access,” he said.
What Actions Can Medical Stakeholders Take?
Health equity should be a “desirable goal” for patients who experience health disparities, but it needs to be a “continuous effort,” Wells said. Focusing on the “how” of eliminating disparities should be a focus rather than checking a box.
Pharmacoequity is also a component of health equity, according to Wells. Where a person lives can affect their health based on their neighborhood’s level of air pollution, access to green space, and food deserts, but where a person lives also affects what parts of the health system they have access to, according to an editorial published in Circulation: Cardiovascular Quality and Outcomes. When patients aren’t taking their medication, it might be because that person doesn’t have easy access to a pharmacy, noted Wells. “It really kind of blows you away when you look at the data.”
Different stakeholders in medicine can tackle various aspects of this problem. For example, healthcare organizations and medical schools can make long-term commitments to prioritizing health equality, Wells said. “You want to make this a part of your practice, your group, or your university. And then once you get a process in place, don’t just check that box and move on. You want to see it. If you haven’t reached your goal, you need to revamp. If you met your goal, how do [you] improve upon that?”
Medical schools can also do better at improving misconceptions about patients of different races and ethnicities. Wells cited a striking paper published in Proceedings of the National Academy of Sciences of the USA that compared false beliefs in biological differences between Black and white people held by white laypeople and medical students. The study found that 58% of laypeople and 40% of first-year medical students believed that Black people have thicker skin than white people. “It’s absolutely amazing when you think about what medical schools can do,” he said.
Increased access to care is another area for improvement, Wells noted. “If you take people who are uninsured and you look at their health once they get Medicare, the gaps begin to close between the different races.”
In terms of individual actions, Wells noted that researchers and clinicians can help to make clinical trials better represent the overall population. At your practice, “treat all your patients like a VIP.” Instead of being concerned about the cost of a treatment, ask “is your patient worth it?”
“I have one of my patients on Medicaid. She’s on a biologic drug. And one of the VPs of my hospital is on the same drug. We don’t treat them any differently.”
The private sector is also acting, Wells said. He cited Novartis’ pledge to partner with 26 historically Black colleges to improve disparities in health and education. “We need to see more of that done from corporate America.”
Are There Any Short-Term Solutions?
Eric Ruderman, MD, professor of rheumatology at Northwestern University, Chicago, commented that institutions have been forming committees and focus groups, but “not a lot of action.”
“They’re checking boxes,” he said, “which is very frustrating.” What can rheumatologists do in the short term, he asked?
Wells noted that there has been some success in using a “carrot” model of using payment models to reduce racial disparities. For example, a recent study analyzing the effects of the Comprehensive Care for Joint Replacement model highlighted the need for payment reform that incentivizes clinicians to spend wisely on patient treatment. Under a payment model that rewards clinicians for treating patients cost effectively, “if I do a great job cost effectively, I could just have more of that money back to my group,” he said.
This article originally appeared on MDedge.com, part of the Medscape Professional Network.
Source: Read Full Article
