A combined treatment strategy targeting SARS-CoV-2 symptoms and severe lung tissue injury is essential to minimize lung sequelae—chronic complications resulting from COVID-19 infection, according to a review published this week in Clinical Microbiology Reviews, a journal of the American Society for Microbiology.
Therapy using lung epithelial stem and progenitor cells shows promise for mitigating the potentially lethal and highly damaging virus-induced inflammatory storm that can occur in severe cases of COVID-19, said Huaiyong Chen, Ph.D., principal investigator at Tianjin Institute of Respiratory Diseases, and Director of Tianjin Key Laboratory of Lung Regenerative Medicine, Haihe Hospital, Tianjin University, China.
“To minimize the damage to the lung, we should promote tissue regeneration efficiently by activating surviving lung stem and progenitor cells, or else by directly transplanting healthy lung stem and progenitor cells into damaged lungs,” said Chen.
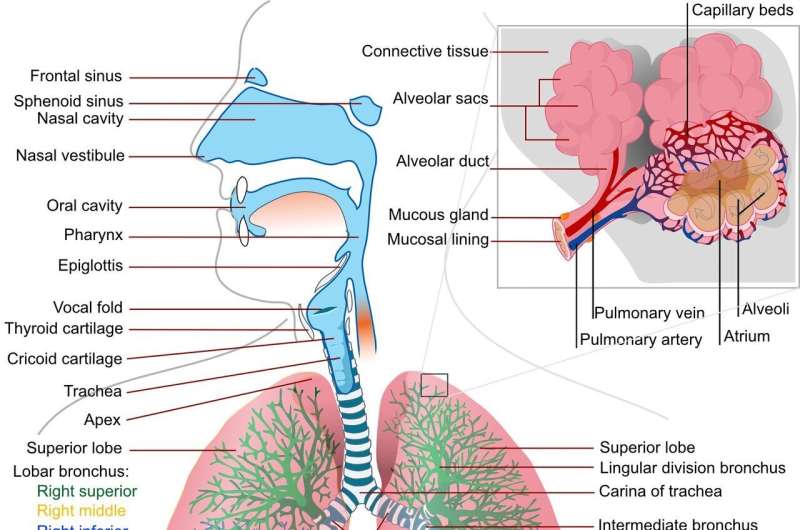
Both cell types can differentiate into lung epithelial cells, which cover the inner surfaces of the lungs where air exchange occurs. In so doing, they can repair lung damage caused by SARS-CoV-2, including fibrosis.
The first step towards activating these regenerative cells is to prime the tissue environment with mesenchymal stem cells. These cells do not normally reside in the lung, but when transplanted there, they secrete growth factors that support the growth and differentiation of the lung epithelial stem and progenitor cells. That, in turn, can repair the damage. The investigators are currently using animal models to figure out how best to accomplish this.
But in severe cases, these regenerative cells may be damaged by cytokines, which are produced by immune cells in excessive numbers during lung inflammation, preventing full restoration of lung structure and function. In such cases, healthy stem and progenitor cells might have to be transplanted into a person’s lungs. However, as with any transplant, immune rejection is likely to be a problem. It may be possible to use gene editing technology, known as CRISPR, to modify these cells to reduce immunogenicity prior to transplantation, a possibility Chen is investigating.
For less severe cases, researchers will need to screen for compounds that boost the capacity of progenitor and stem cells to trigger repair and regeneration of lungs following these injuries. Previous research has shown that certain compounds that target signaling pathways in stem and progenitor cells show potential for enhancing lung regeneration in patients with asthma and lung fibrosis. They may do likewise for SARS-CoV-2 patients.
Source: Read Full Article
