Breathing difficulties mark a rare form of autism. Now, UConn researchers have traced the symptom to a specific set of brain cells—and possibly found a way to help sufferers.
Pitt Hopkins syndrome is very rare, affecting perhaps 250 people in the world right now. One of its defining features is forced hyperventilation, followed by breath-holding. It also seems that people with Pitt Hopkins syndrome are unable to actively exhale.
“It’s really disruptive for the person, and can make them sick. Aspiration-induced pneumonia is a leading cause of death for people with Pitt Hopkins,” says UConn neurobiologist Dan Mulkey, associate professor in the Department of Physiology and Neurobiology. “Despite this, we know virtually nothing about how the disease disrupts breathing.”
From a genetic point of view, people with Pitt Hopkins syndrome are missing a specific gene on their 18th chromosome that encodes for transcription factor 4 (Tcf4). Transcription factors help turn other genes on or off. So people with Pitt Hopkins have the syndrome because Tcf4 isn’t around to turn the right genes on or off. But while the lack of Tcf4 appears to be the cause, doctors and researchers don’t know what Tcf4 does under normal conditions. So they do not understand why loss of this gene causes breathing difficulties as well as other problems including intellectual disability, developmental delays, and seizures. And that makes it very difficult to find a treatment.
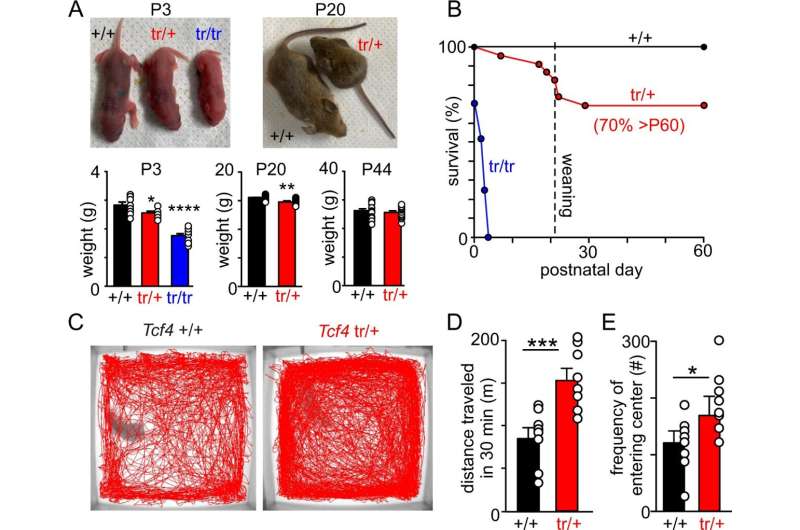
Mulkey and his students looked at mice missing Tcf4 to see if they could figure out more about the syndrome. The mice show key features of Pitt Hopkins, including frequent bouts of hyperventilation followed by breath-holding. Zooming in on the part of the brainstem that controls breathing, the team found a very curious thing. A group of cells some scientists had thought might control expiration (the process of breathing out) were mostly missing. This was the first time those cells had ever been implicated in a breathing disease, and it adds further evidence that they really are important for exhalation. Another group of cells nearby that are known to control inspiration (breathing in) weren’t functioning normally, and their ability to communicate with other parts of the brain’s respiratory system was altered, as if the breathing circuit was mis-wired.
“We discovered a complete shift in how these cells connect to each other. And we don’t know what it means. This was entirely unexpected. Together these unexpected findings suggest Tcf4 is required for development and normal function of inspiratory and expiratory neurons,” Mulkey says. In other words, Tcf4 regulates the brain cells that regulate breathing.
And there was something else strange in the brainstems of the mice: there was a sodium channel in the cells that wasn’t supposed to be there. Sodium channels help nerve cells get excited and fire off signals to one another. The out-of-place sodium channel they found is usually expressed only by peripheral nerve cells and other parts of the body, never inside the brain.
The sodium channel seemed like a clue. The researchers tried giving the Pitt Hopkins mice a blocker of this sodium channel. Several of the symptoms of the syndrome improved, including the breathing abnormalities as well as hyperactivity. But another sodium channel blocker that cannot enter the brain did not improve the symptoms. Finally, the Mulkey team also used a genetic approach to knock down expression of that sodium channel only in breathing-related brain cells, and this also improved the mice’s symptoms. These results will be published in the October 13 issue of Nature Communications.
Source: Read Full Article
